Calling all clinicians: Survey on ocular disfigurement
Optometrists, ophthalmologists and eyecare clinician-scientists are being asked for their input in a short, anonymous survey on ocular disfigurement and the use of scleral shell prostheses in New Zealand.
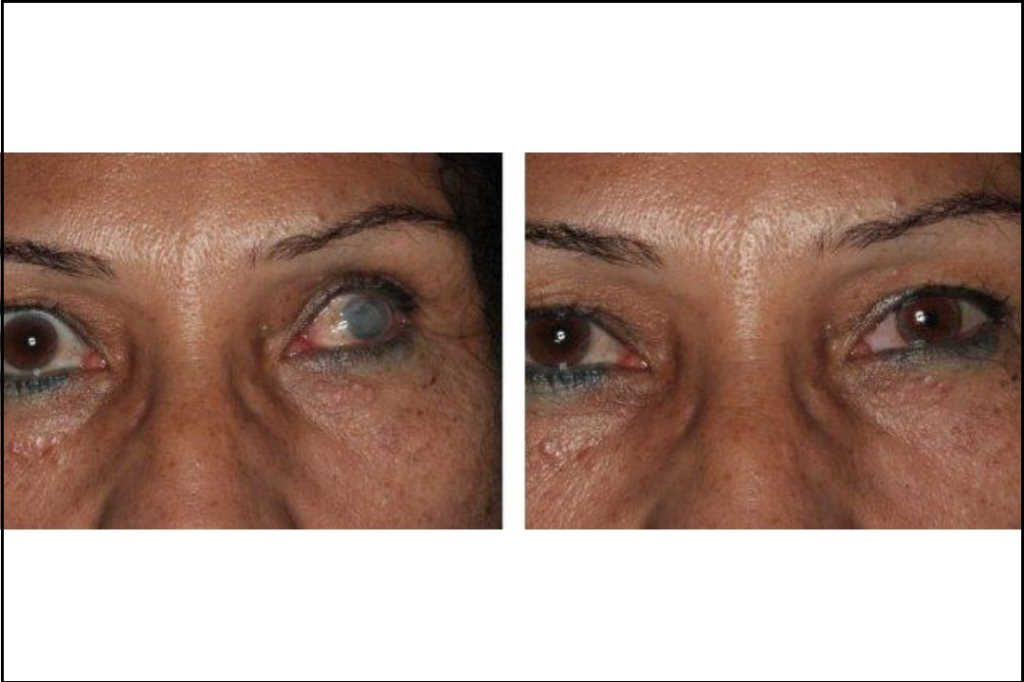
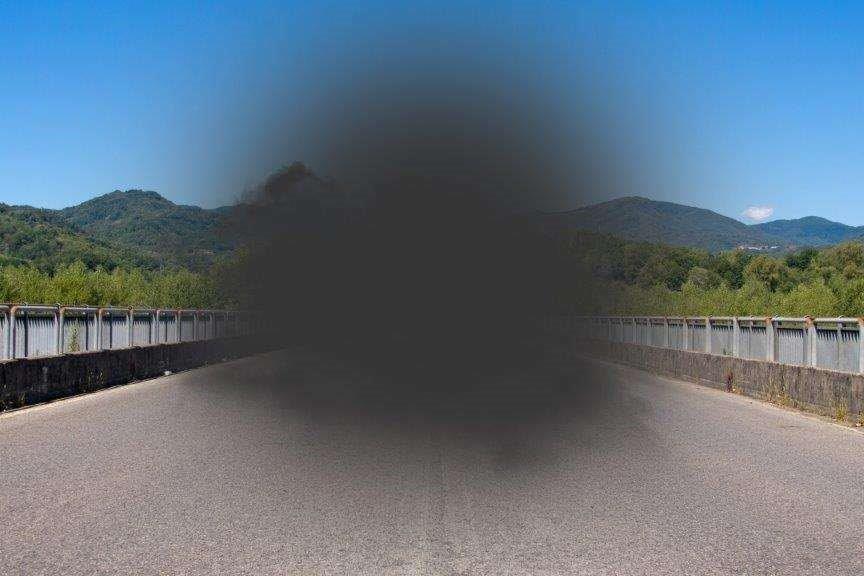
Despite the well-recognised cosmetic, functional and quality of life improvements associated with ocular prosthetic rehabilitation following eye loss or disfigurement, there is a paucity of peer-reviewed research on the subject, said Auckland University PhD candidate Janice Yeoman. “In particular, there is minimal clinical research on scleral shell prostheses, a sub-type of ocular prosthesis designed to be fitted over non-functional, disfigured eyes.”
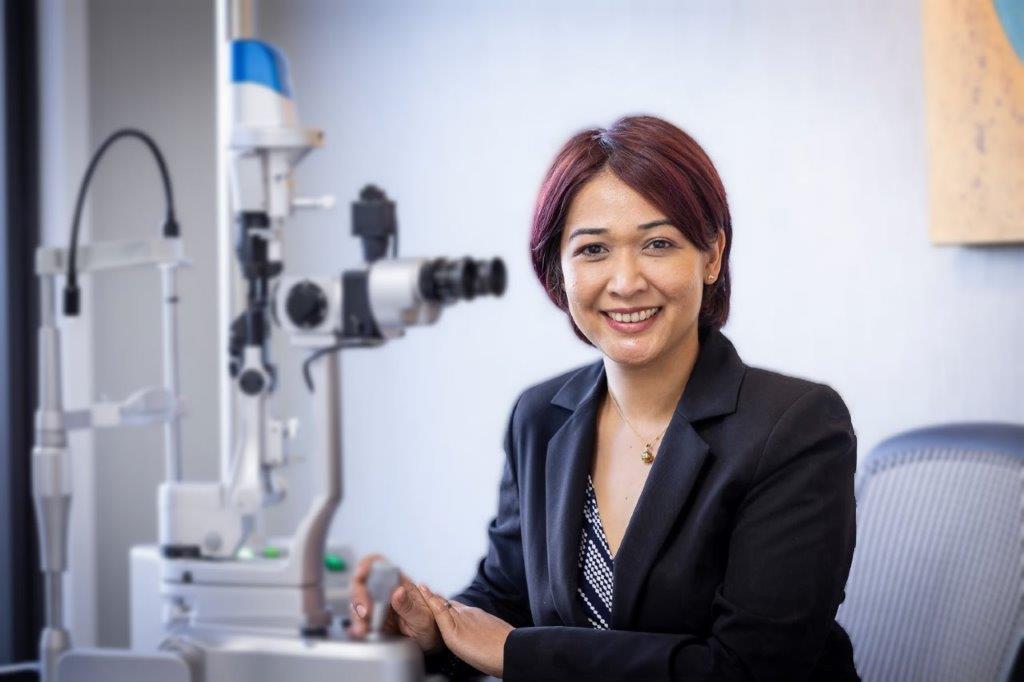
Yeoman and her university supervisors, optometrist-scientist and senior lecturer Dr Stuti Misra and oculoplastic ophthalmologist Dr Brian Sloan, are investigating the epidemiology of ocular disfigurement in New Zealand, the concerns and experiences of those affected and current practices around prosthetic rehabilitation. In New Zealand it is estimated that 1 in 9000 people wear a scleral shell prosthesis, but it’s suspected that many more may benefit from this prosthesis. “As scleral shell prosthesis use gains favour and there are efforts to make scleral shells more accessible, there is a growing need for evidence-based information on their indications for use, wearing, cleaning and fitting practices, and effects on ocular surface physiology. More information is needed to predict cases in which scleral shell use will be successful and how to manage cases and improve outcomes in cases where comfort and tolerance are sub-optimal.”
This is the first study of scleral shell wearers and practice in New Zealand, said Yeoman. “The input of all ophthalmologists, optometrists and eyecare clinician-scientists is crucial to providing an understanding of current practices. Even if they don’t assess patients with ocular disfigurement and scleral shells very often in practice, their input is requested.”
The survey will provide context for the overall research, which will also include clinical assessments to understand the relationships between ocular surface morphology and physiology, dry eye, scleral-shell fitting techniques, maintenance practices and comfort in shell wearers. These findings will assist clinicians from all fields in providing evidence-based care to New Zealanders affected by ocular disfigurement in the future, said Yeoman and Dr Misra.
To access the clinician participant information and take part in the survey, please go to https://auckland.au1.qualtrics.com/jfe/form/SV_d0hfR9hEp8iVaqq.