Considering surgical interventions and glaucoma
Long-term effect of YAG laser iridotomy on corneal endothelium in primary angle closure suspects
Liao C et al
Br J Ophthalmol 2021;105:348–353
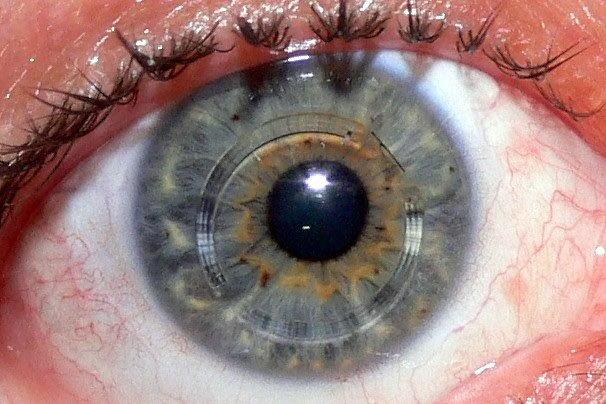
Review: This study evaluated the impact of YAG laser peripheral iridotomy (LPI) on corneal endothelial cell density (ECD) and morphology in primary angle closure suspects (PACS) over a 72-month period.
A total of 875 patients were included in the study, with one eye receiving YAG LPI and the fellow eye serving as a control. The study found ECD declined significantly over time in both the treated and untreated eye (p<0.001). Eyes treated with YAG PI showed more progressive cell loss with increasing time (p<0.001). There was not a significant difference in amount of ECD loss between treated and fellow eyes until the 72-month follow up (4.9% in LPI eyes vs 4.2% in non-LPI eyes, p=0.003). No significant correlation to explain ECD loss in the in LPI-treated eyes was found between age, gender, ocular biometrics, intraocular pressure and laser settings, except for time effect (p<0.01).
Comment: LPI is the conventional first-line treatment for individuals with primary angle closure. While LPI is generally felt to be safe, there have been reports of corneal complications including oedema and decompensation post iridotomies. This study introduces the possibility that with time, YLI may further exacerbate the loss of ECD seen with age. While the exact mechanism for this loss is only theoretical (changes aqueous humor dynamics), the question remains whether this difference continues to significantly change as time passes. Further, as many of these patients go on to require cataract surgery at some point in their lifetime, a procedure already documented to impact ECD, are these patients then at risk of a cumulative loss of ECD and hence exposed to the potential for increased risk of decompensation long term?
Three-year outcomes of second-generation trabecular microbypass stents (iStent Inject) With phacoemulsification in various glaucoma subtypes and severities.
Salimi A et al
J Glaucoma 2021;30:266–275)
Review: This single-centre longitudinal case series looked to assess the three-year effectiveness and safety profile of iStent Inject second-generation trabecular microbypass stent implantation with concomitant cataract surgery in eyes with glaucoma.
A total of 124 eyes with different glaucoma subtypes and severities were included. At three years mean intraocular pressure (IOP) was reduced by 22% (P<0.001) (16.9 mmHg to 13.17mmHg). The mean number of medications was reduced by 51% (P<0.001) postoperatively (2.38 to 1.16 medications). 76% of eyes eliminating ≥1 medication and 37% of eyes eliminating ≥2 medications. At three years, 96% of eyes achieved IOP ≤18mmHg (vs. 69% preoperatively), 80% of eyes achieved IOP ≤15mmHg (vs 40% preoperatively), and 42% of eyes achieved IOP ≤12mmHg (vs. 7% preoperatively). Post-phacoemulsification cup-to-disc ratio, visual field (VF) mean deviation, and RNFL and GCIPL thickness remained stable.
Comment: This study demonstrated a sustained and significant IOP and medication reduction, with a good safety profile observed over three years across all glaucoma subtypes and severities. MIGS procedures, from inception, offered the appeal of having a good benefit-risk profile when compared to more traditional filtration surgery.
Patient selection is extremely important when considering MIGS devices. The authors explain that the i-stent is suited to patients whose disease does not necessitate a dramatic IOP reduction. This study suggests, that in the appropriate patients, iStent Inject could be a durable, consistent and safe minimally invasive surgical intervention to consider in the arsenal of the glaucoma surgeon.
Glaucoma-related central VF deterioration after vitrectomy for epiretinal membrane: topographic characteristics and risk factors.
Tsuchiya S et al
Eye 2021; 35:919–928
Review: This study sought to identify risk factors for glaucoma-related central VF deterioration after vitrectomy with internal limiting membrane (ILM) peel for epiretinal membrane (ERM).
The eyes of 33 patients with and without glaucoma who underwent vitrectomy with ILM peel for ERM were analysed and Humphrey 10–2 VFs and ganglion cell complex (GCC) thickness were measured at baseline, three, six and 12 months postoperatively. VF mean deviation significantly deteriorated postoperatively only in the eyes with glaucoma (P<0.001). Older age, longer axial length, pre-operative worse mean deviation (ie. worse glaucoma) and thinner GCC were all found to be significant risk factors for postoperative deterioration. Sector-wise analysis revealed that total deviation in the superior/inferior outer arcuate sectors significantly deteriorated only in the glaucoma group. Pre-operative worse total deviation and thinner GCC were significant risk factors for deterioration in the superior outer-arcuate sector.
Comments: Previous studies have introduced the concept that PPV may cause VF loss and PPV with ILM peel for ERM may result in VF deterioration in patients with coexisting glaucoma. This study goes onto add that the central VF within 10⁰, especially in the outer-arcuate sectors, deteriorated post procedure in eyes with glaucoma, while it remained stable in eyes without glaucoma. It also identified that worse VF and thinner ganglion cell complex were predictors of postoperative central VF worsening. The results of this study suggest that careful consideration needs to be taken when considering management of ERM in patients with pre-exisiting glaucoma and that eyes with advanced glaucoma are at higher risk of postoperative central VF deterioration.
Dr Kaliopy Matheos is a consultant ophthalmologist and subspecialist in glaucoma and cataract at Greenlane Hospital (ADHB) and in private practice at Eye Institute, Auckland.