Papilloedema in kids, AMD, PED and more
A warm summer evening and the lure of the beach or BBQ were not enough to deter attendance at the Eye Doctors’ first Grand Round in February at the Novotel Ellerslie, Auckland. The four presenting ophthalmologists gave the full house plenty to think about and, together with the CPD points and networking on offer, made up for any aforementioned activities.
An international perspective
Newly-returned from overseas, Dr Penny McAllum said her overall conclusion post-travels was our health system “isn’t perfect and we have limited resources … but we’re doing okay!”
In Scotland, she met Dr Sathish Srinivasan and observed a fascinating-sounding trial of RxSight’s light-adjustable IOLs, she said. After implantation, patients were released wearing wrap-around dark glasses. The lenses were adjusted over the next few weeks until deemed correct and then “locked in” by setting with a special light.
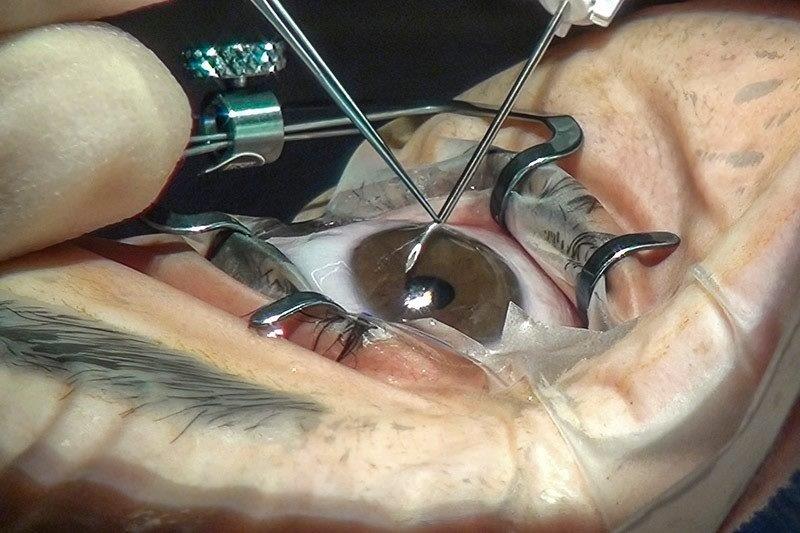
In Nottingham, Dr McAllum met Professor Harminder Dua, who controversially described the eponymous Dua’s layer in 2013. His current work includes deep anterior lamellar keratoplasty (DALK) using big bubble (BB). Type 1 BB makes up 80% of cases and is done between the stroma and Dua’s layer, with an 8-9mm very strong and central bubble, she explained. Type 2 BB is done between Dua’s layer and DM, with a 10mm bubble where the weak posterior lamella is smoother but more easily torn. Prof Dua found Type 1 BB was associated with a lower incidence of conversion penetrating keratoplasty (PK) (0% vs 75%) and also gave better visual results than either Type 2 or a mixed type.
Dr McAllum came to the conclusion that the UK’s National Health System (NHS) is generally similar to our own public system, but its method for selecting patients for cataract surgery seemed more objective, she said. The UK selection process is based on optometrist referrals, while in some centres the health service also operates a “one-stop shop for straightforward cataract surgery”, treating all patients almost entirely with topical anaesthetic. Dr McAllum was also impressed with the NHS’s emphasis on team structure and collaborative care and what she felt was a more engaged, collegial and relaxed atmosphere.
Another notable stop on Dr McAllum’s itinerary was Noida on the outskirts of New Delhi, India, where she met Dr Mohita Sharma, the recipient of the 2017 Women in Ophthalmology honorary lecture award who has now established an 800-member-and-growing network for female ophthalmologists in India. She was dismayed, however, to discover only 30% of specialist doctors in India work in the public sector. While superficially similar, she found some Indian practices disconcerting, such as having more than one patient in theatre at the same time.
She concluded her international observations noting elephants are very prone to conjunctivitis and keratitis and 60% of Indian and 25% of Sri Lankan elephants have corneal opacities.
DD vs papilloedema
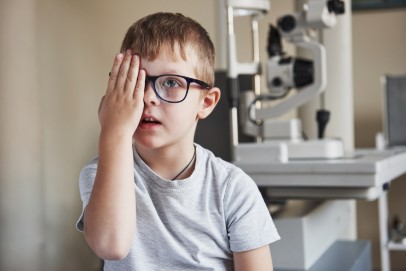
Next up was the newest member of the team (see box story) Dr Julia Escardo-Paton who discussed the differences between optic disc drusen (ODD) and papilloedema, especially in children.
Since the Vincent Barker landmark case – where an optometrist was publicly vilified for failing to spot papilloedema in an eight-year-old boy who later died – there has been a deluge of referrals of children with “swollen discs”, especially in the UK, she said.
Key is better education for optometrists, ophthalmologists and paediatricians, and good history taking and assessment of both optic discs and risk, said Dr Escardo-Paton. Behavioural changes are very important as a child may not provide enough information when taking a history and symptoms may differ from those in an adult. She also suggested taking a picture to study rather than trying to get a child to sit still.
In children, papilloedema can be asymptomatic or unilateral; children with optic drusen only may get normal headaches; papilloedema can coexist with drusen; and in young children, drusen may not yet be calcified, however, drusen was far more likely than papilloedema, she said.
Dr Escardo-Paton assessed the strengths and limitations of disc imaging modalities, saying stereo disc photos were essential for virtual clinics but not always readily available and, while it was the gold standard for drusen, an ultrasound B-scan will not detect uncalcified drusen. OCT was good for monitoring but not diagnosing and, despite their usefulness, fluorescein angiograms required resources such as the presence of a paediatric nurse and may not detect buried drusen.
When in doubt, use multiple imaging modalities and refer for paediatric investigations, such as blood tests, CT/MRI and/or lumbar puncture. Finally, in these cases, continue to monitor the patient’s optic nerve function and check with regular stereo disc photos and OCT, she said.
An unusual case and recent papers
Dr Mark Donaldson presented “a case and a paper”. He described a patient who presented to optometry with a black spot in the vision of their left eye, noticed since waking, and was referred for ophthalmic assessment. The patient had a significant cardiovascular history and on examination, an embolus and an Hollenhorst plaque were found in the temporal circulation of the left retina. He was immediately admitted to the stroke unit at Auckland Hospital, where four days later he had a stroke preventing left carotid endarterectomy.
The paper was Australian age-related macular degeneration (AMD) specialist Professor Robyn Guymer’s on the LEAD trial which showed sub-threshold nanosecond laser (SNL) treatment appeared to make no significant difference in the overall progression rate of participants with intermediate AMD without signs of late AMD. The paper concluded, however, SNL may play a role in slowing progression for those without coexistent reticular pseudodrusen (RPD) and may be inappropriate in those with RPD. The authors stressed the findings should not be extrapolated to other laser drusen treatments.
In conclusion, Dr Donaldson highlighted the results of another study showing photobiomodulation (PBM) therapy reduced drusen volume and improved visual acuity and contrast sensitivity in a cohort of dry AMD subjects. PMB is a non-laser, long wavelength diode light treatment.
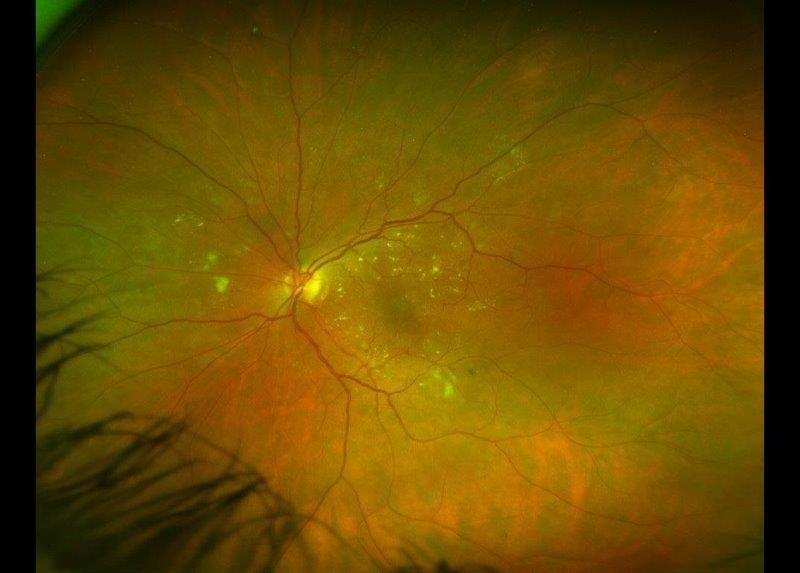
Pigment epithelial detachment
The final speaker for the evening, Dr Andrew Riley focused on pigment epithelial detachment (PED), showing how to recognise different types with OCT and discussing whether PED should be treated, which depended on the cause. For choroidal neovascularisation (CNV) with leak, always treat; for central serous chorioretinopathy (CSCR), sometimes treat; serous PED, not usually; and no treatment for fibrovascular scar or vitelliform lesion.
Treatment included anti-VEGFs, with Dr Riley giving Eylea the thumbs up in comparison with others, carbonic anhydrase inhibitors, steroids and phosphodiesterase inhibitors. Sildenafil (Viagra), he said, was effective in increasing choroidal circulation. Counselling patients that smoking tripled the risk of AMD, while a good diet and supplements were beneficial.
New Eye Doctor
Dr Julia Escardo-Paton is the latest addition to Eye Doctors replacing Dr Shuan Dai, who was lured across the ditch late last year. Like Dr Dai, Dr Escardo-Paton specialises in paediatric ophthalmology, strabismus in adults and children and general ophthalmology, including cataracts.
After growing up in Peru and Venzuela, Dr Escardo-Paton graduated from university in the US, before undertaking medical school and post-graduate training in the UK.
She gained fellowships in paediatric ophthalmology and strabismus in Bristol and Auckland, and subsequently worked as a consultant ophthalmologist in both those fields in Wales. She returned to Auckland in 2017, taking up a paediatric ophthalmology role with Counties Manukau and then focusing on adult strabismus and retinopathy of prematurity with the Auckland District Health Board.