CASE STUDY: Optimising outcome in non-exudative AMD
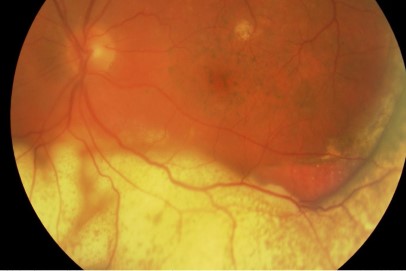
A 68-year-old man has been under my care for age-related macular degeneration (AMD). His right eye is under long-term anti-VEGF therapy for wet AMD. He has non-exudative (dry) AMD in his left eye and wanted to know if there was anything he could do to improve the outcome for his left eye. His visual acuity was 6/9 right and 6/12 left. The optical coherent imaging of his left macula is shown in Fig 1.
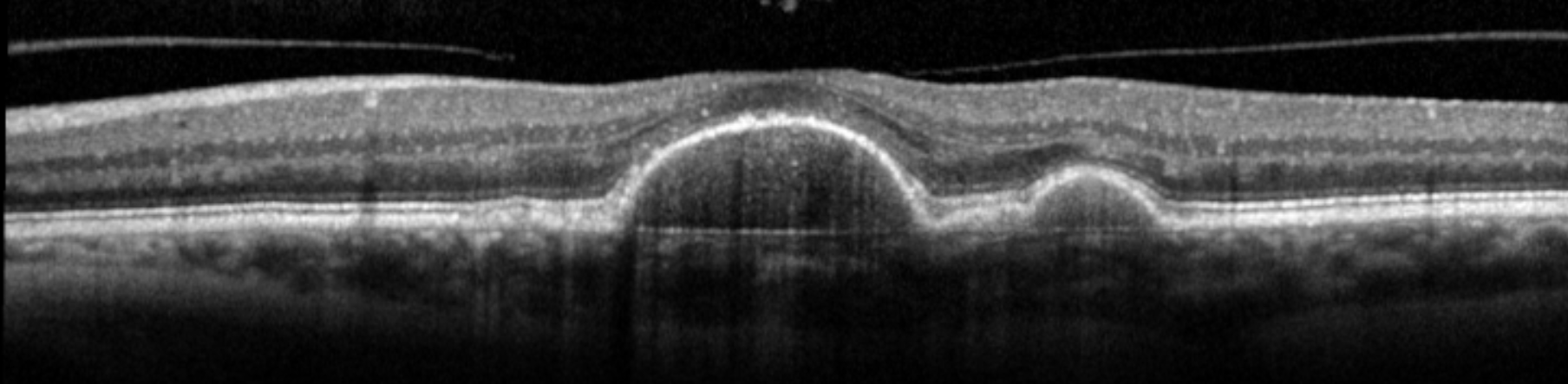
Fig 1. OCT of the patient’s left macula
AMD is a common disease among older people. Overall, the prevalence of AMD in the population 40 years or older is 6.5%, with the prevalence of geographic atrophy (GA) or neovascularization in 1.47%1. The prevalence of AMD increases with age. As a result, it is not uncommon that patients with non-exudative AMD present with concerns regarding their vision. Often, they want to do all they can to prevent disease progression to late AMD, preserve their vision and avoid intravitreal injections. Treatment for this group of patients is limited and many have been told that ‘there is nothing else one can do for dry AMD’. However, there are a number of new developments that will benefit these patients.
Accurate risk assessment using OCT
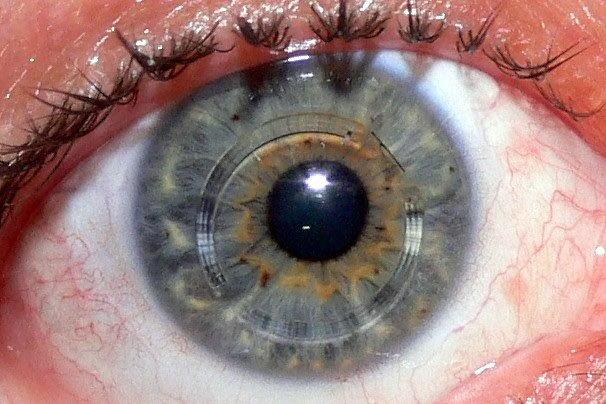
It is essential to obtain an accurate assessment of the risk of progression to advanced AMD in these patients. Traditionally, risk assessment is performed by slit lamp biomicroscopy or colour fundus photos. Using an OCT to take images of the macula for assessment, however, is now the preferred and my preferred method to assess progression risks.
Four OCT biomarkers have been found to be predictive of progression to late AMD. In order of importance, these are hyperreflective intraretinal foci, hyporeflective foci in drusen, reticular pseudodrusen and increased drusen volume2,3.
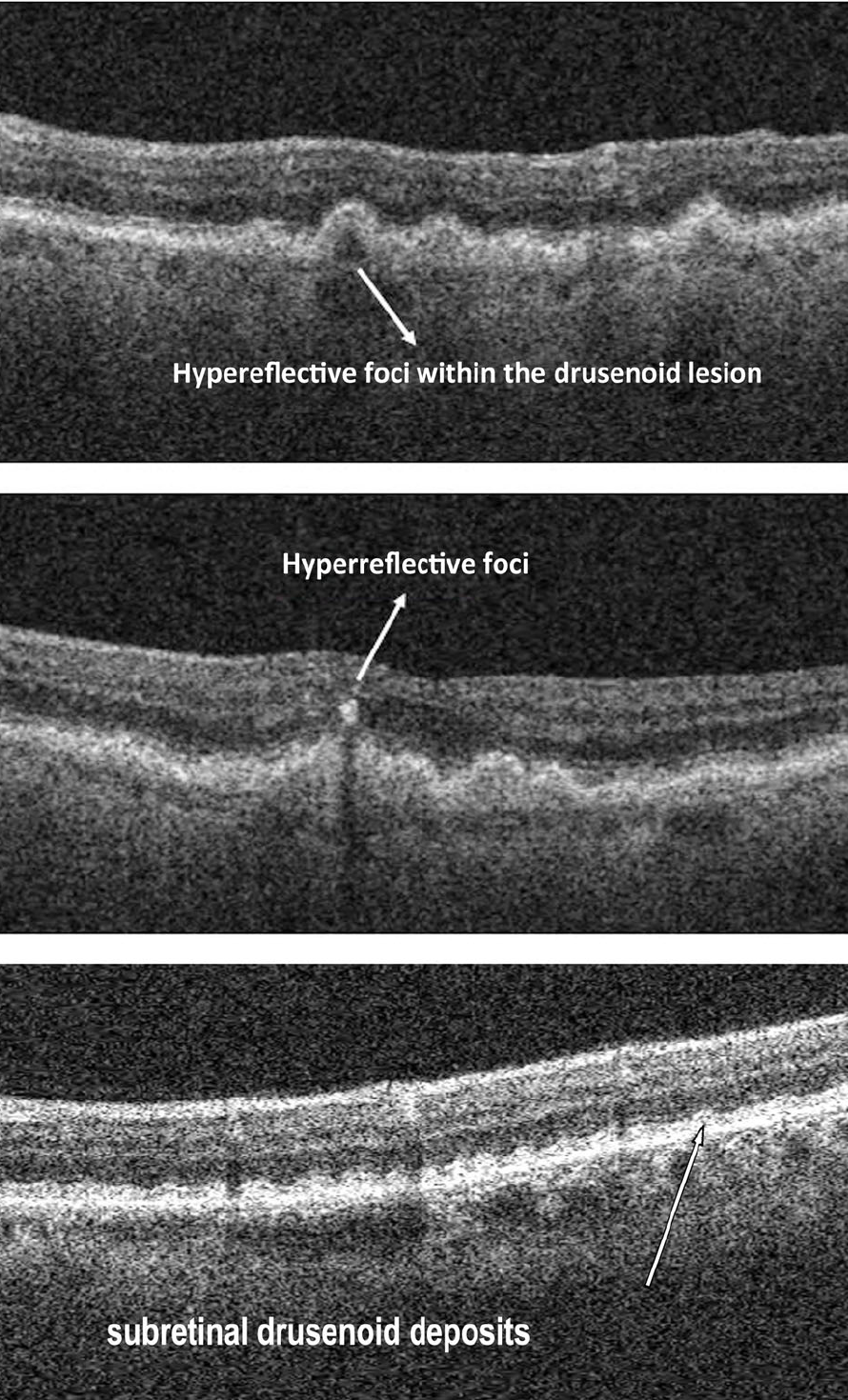
Fig 2. OCT biomarkers for progression, from Lei et al3
|
Hazard ratio for progression to late AMD |
|
|
Hyperreflectivce intraretinal foci |
5.21 |
|
Hyporeflective foci in drusen |
2.42 |
|
Reticular pseudodrusen |
1.95 |
|
Drusen volume > 0.03mm3 |
1.46 |
Table 1. Hazard ratio for second eye AMD progression (first eye already affected by exudative AMD with macula neovascular membrane)2
Modifying ongoing risks
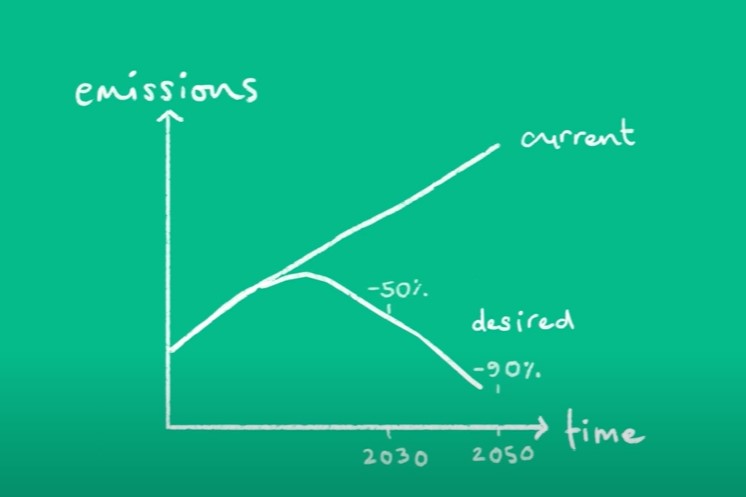
Traditionally, there is little one can do to prevent progression of AMD apart from smoking cessation and AREDS2 nutritional supplementation. However, the 2RT laser (Ellex) represents an exciting development in AMD research.
The recently published, Subthreshold nanosecond laser intervention in AMD: the LEAD randomised controlled clinical trial provides some high-quality data on the effectiveness of 2RT laser in preventing the development of late AMD4. In this study, 292 patients with large drusen without atrophy were randomised to receive 2RT laser treatment or sham. Overall, the study did not show a beneficial effect for the 2RT laser (hazard ratio 0.61 for progression, p=0.122). However, 76% of the participants in this study had drusen without reticular pseudodrusen and in this patient group a significant slowing of progression rate (hazard ratio 0.22, p=0.002) was observed with 2RT treatment. Interestingly, for the remaining 24% of the participants with reticular pseudodrusen, there was a worsening of progression rate (hazard ratio 2.56, p=0.112) with 2RT treatment.
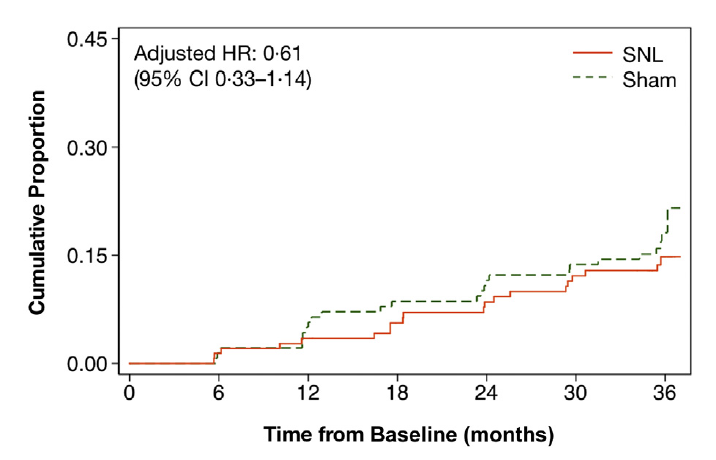
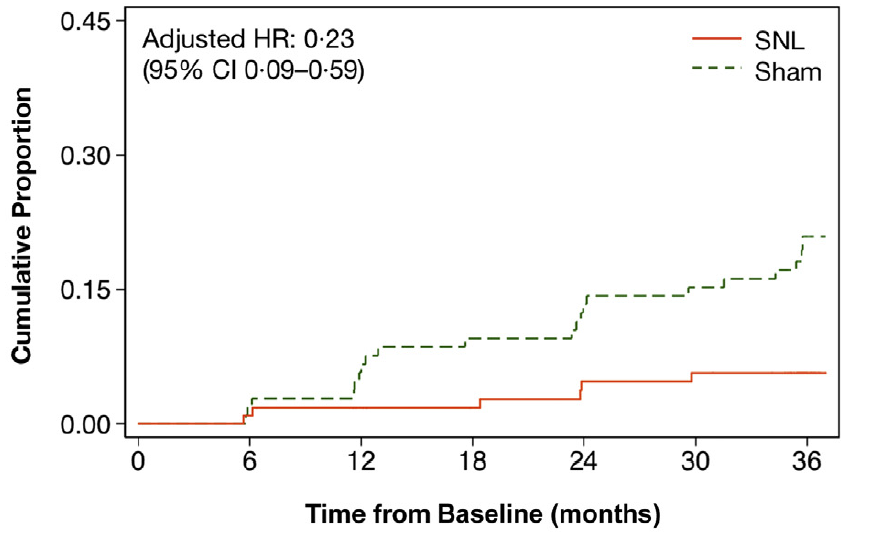
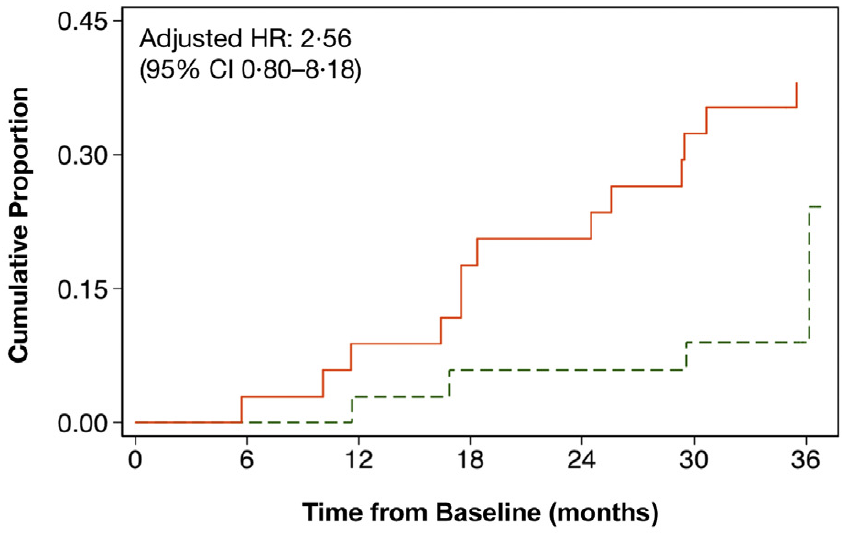
Fig 3. Kaplan-Meier failure plots summarising LEAD study results4
Interpreting these results
Clinicians are right to be cautious. Many ophthalmologists argue that 2RT should not be used in the management of non-exudative AMD, even in cases without reticular pseudodrusen, as the main result of the trial was negative and the subgroup analysis was performed post hoc, despite the significant results. On the other hand, non-exudative AMD is a progressive disease (clearly demonstrated by the sham group in this study).
Unfortunately, further data will not be forthcoming in the near future as this will involve a further randomised controlled study with a significant follow-up period, and many patients with non-exudative AMD will have progressed to advanced AMD while waiting for better data. Furthermore, the 2RT laser treatment is already available in New Zealand and patients should be given the opportunity to make up their own mind about this treatment guided by research data.
It is my personal opinion, however, that 2RT laser treatment should not be offered to patients with reticular pseudodrusen as there is evidence of harm. But a careful discussion on 2RT laser, especially regarding the trial result, is warranted for those with drusen without reticular pseudodrusen. Although the post hoc analysis is very suggestive of a benefit in this subgroup, the result is definitely not conclusive, so these patients need to make up their own mind regarding 2RT treatment. I do not believe 2RT laser treatment should necessarily be withheld if the patient has been given objective data on the treatment and made an informed decision to pursue treatment. Once there is OCT evidence of GA (including nascent GA), there is no evidence that 2RT laser will be beneficial.
Both reticular pseudodrusen and nascent GA are subtle features on OCT. It is best for these patients to be seen by a medical retina specialist prior to considering 2RT laser treatment.
Early detection and treatment for exudative AMD
Conversion to exudative (or neovascular) AMD remains an important threat to vision loss in this group of patients, especially if the conversion is detected late. All patients with non-exudative AMD should be given an Amsler grid and asked to monitor their monocular vision at least once a week. Rapid access to ophthalmology assessment with OCT imaging and urgent treatment with anti-VEGF injections are necessary to preserve central vision. So, as OCT imaging becomes more available, community optometrists play an important role in the early detection of macula neovascularization, and a collaborative approach between optometrists and ophthalmologists is essential for a good outcome.
Novel treatments for atrophic AMD
For those patients unfortunate enough to develop GA, there are some novel treatments on the horizon that may help to prevent disease progression. A phase II study looking at intravitreal injection of an inhibitor of C3 in the complement system showed this molecule is effective in slowing the progression of GA5. A multi-centre international phase III study is now underway and the result is expected within the next two to three years. If this phase III study is positive, GA may become a treatable disease.
In summary
There are a number of developments in the management of non-exudative AMD and the risk of AMD progression can now be assessed accurately with OCT. 2RT laser has the potential to transform the treatment of non-exudative AMD, though further data is required to prove its effectiveness. Early detection of neovascular disease remains an important strategy in preventing vision loss and community optometrists have a crucial role to play in this area. While GA may become a treatable disease with C3 inhibition.
As a medical retina specialist, I am excited about recent developments within my field and I am looking forward to guiding patients through these novel and promising strategies.
References
1. Klein, R. et al. Prevalence of age-related macular degeneration in the US population. Arch. Ophthalmol. Chic. Ill 1960 129, 75–80 (2011).
2. Nassisi, M. et al. OCT Risk Factors for Development of Late Age-Related Macular Degeneration in the Fellow Eyes of Patients Enrolled in the HARBOR Study. Ophthalmology (2019) doi:10.1016/j.ophtha.2019.05.016.
3. Lei, J., Balasubramanian, S., Abdelfattah, N. S., Nittala, M. G. & Sadda, S. R. Proposal of a simple optical coherence tomography-based scoring system for progression of age-related macular degeneration. Graefes Arch. Clin. Exp. Ophthalmol. 255, 1551–1558 (2017).
4. Guymer, R. H. et al. Subthreshold Nanosecond Laser Intervention in Age-Related Macular Degeneration. Ophthalmology 126, 829–838 (2019).
5. Liao, D. S. et al. Complement C3 Inhibitor Pegcetacoplan for Geographic Atrophy Secondary to Age-Related Macular Degeneration. Ophthalmology 127, 186–195 (2020).
Dr Leo Sheck is a consultant ophthalmologist with the Auckland District Health Board and Eye Institute. Specialising in medical retina, genetic eye disease, electrodiagnostics for complex retina and optic nerve diseases and cataract surgery, especially with co-existing retinal diseases, he is also chair of the New Zealand Save Sight Society.