Comment: YAG laser optometry scope change
As a hospital-based optometrist, I was very excited to hear of the recent Optometrists and Dispensing Opticians Board’s decision to approve a new scope of practice for hospital-based optometrists in ophthalmic laser surgery and its associated prescribing qualification. This is a major milestone for the optometry profession as the new scope will allow trained optometrists to contribute their skills and knowledge in helping to reduce ocular health burdens for New Zealanders by working collaboratively with ophthalmology. I am particularly pleased to note the following:
1. Further training and specialisation
At a personal level, I am excited about the opportunity to receive further training related to ocular health. When optometrists were approved to be glaucoma prescribers, I jumped on board at the first opportunity and was eager to learn as much as I could. I started to attend as many glaucoma conferences as I could (I even flew to Finland!) and set up the Wellington Glaucoma Prescriber Peer Review group. Since then, I have joined the glaucoma team in Wellington and within a supportive environment continue to learn as much as I can about glaucoma. The feeling that there is always more to know and to do is invigorating, and the challenge is compelling. This new scope and prescribing qualification will provide a moment for me to step up yet again in my career – I am always striving to become the best optometrist I can be.
2. Being able to contribute more to my team
In the past two years, I have had the privilege of working alongside an experienced glaucoma optometrist, two supportive glaucoma specialists and a team of amazing nurses, registrars and fellows at Wellington Hospital. Every day I work with them, I feel I am learning and growing as a clinician. Public hospital clinics can be tough and there are days when I feel utterly exhausted by the time I leave, but when I see how hard my colleagues are working beside me it gives me strength and motivation to give each day my best. As a member of such a supportive team, I am thrilled even thinking about the possibility that I will now be able to contribute more to help my colleagues.
3. Provide timely, safe treatment for patients
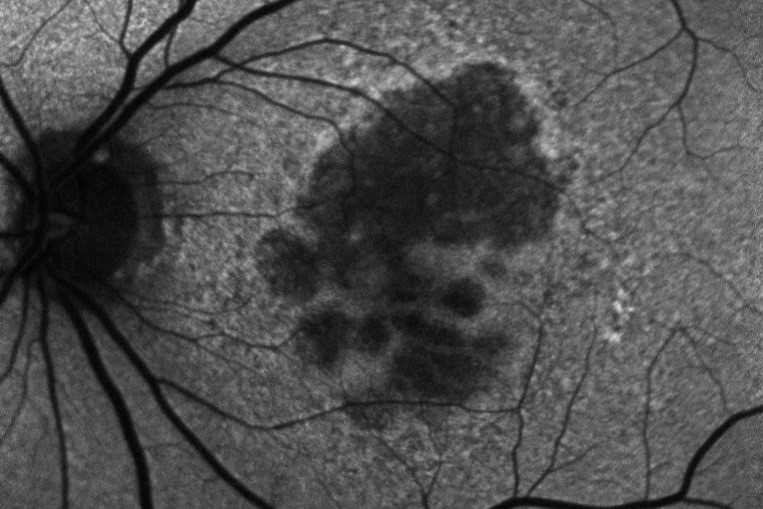
In my clinic, I have to rebook patients into separate laser clinics for them to receive the treatment they need. Posterior subcapsular opacity can significantly reduce a patient’s visual acuity, so being forced to wait for treatment, often for quite a long time, can have a considerable negative impact on our patients’ lives. Now, being able to deal with this quickly and far more conveniently will benefit them immensely and be greatly appreciated. Additionally, I have seen a number of patients needing same-day peripheral iridotomies, typically in a very busy clinic. If, after reviewing the patient with the consultant ophthalmologist, I could safely conduct the procedure myself, the patient would receive timely treatment without waiting to see another clinician, and the overall flow through the clinic would also be less disrupted.
I am aware this scope change will only apply to a small subset of optometrists in New Zealand and will require many hours of training. Yet it is a good move in the right direction. With robust and effective training systems, I have confidence New Zealand can provide the same level (if not better) care for our patients needing laser treatment, matching the safety profiles seen overseas.

Inhae Park is a glaucoma optometrist working in Wellington Hospital and with Capital Eye Specialists.