Keeping an eye out for periocular malignancy
We all look at faces and eyes every day. Be it refracting, screening for diabetic retinopathy, looking for retinal tears or monitoring glaucoma, we are looking closely. But do we see? Do we look for and see the nodular basal cell carcinoma at the medial canthus or the squamous cell carcinoma on the lower eyelid margin?
Lumps and bumps
Lumps and bumps appear relatively commonly in the periocular region, many of them benign and related to the abundance of sweat- and oil-producing glands in this area. As a rule, if the lump has been present a long time, is not growing, does not bleed and there are eyelashes growing through it, it is more likely to be benign (Fig 1). These lesions can be photographed and observed, or easily removed as a clinic-based procedure.

Fig 1. Benign eyelid lesions
John
John was 41 years old and had had a lesion on his right lower eyelid for as long as he could remember (Fig 2). He wanted to know if it was something to be concerned about.

Fig 2. Benign intradermal naevus
His history was not suggestive of malignancy. The lesion had been present for many years, with no ulceration, recent growth or bleeding, and the eyelashes growing through it suggested normal tissue architecture. Such lesions can be photographed and observed or excised for comfort or cosmetic reasons.
Periocular malignancy
New Zealand has one of the highest rates of skin cancer in the Western world. Its geographical position, coupled with the eyes’ anatomical location means the periocular region is exposed to high levels of UV radiation. Consequently, New Zealanders’ eyelids are subject to higher rates of cutaneous malignancy1,2. Risk factors for periocular malignancy include increasing age, fair skin, sun exposure, genetic predisposition, immunosuppression and a history of previous cutaneous malignancy.
If you see a lesion or lump that is firm, has a history of growth or bleeding, has associated dilated blood vessels (telangiectasia), central ulceration or madarosis (loss of eyelashes), these are red flags for malignancy and warrant biopsy. These lumps are not usually painful, and patients may be asymptomatic or have only irritation if the lump interferes with wearing glasses.
Look, see and refer
The ‘big three’ skin cancers arising around and on the eyelids are basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma. Rarer malignancies can arise from specialised eyelid tissues unique to this region, such as sebaceous cell carcinoma arising from the meibomian glands - beware the recurrent chalazion.
BCC is one of the most common cancers in the world and makes up more than 90% of periocular skin cancer1 (Fig 3). BCC is most commonly found on the lower eyelid due to the relative protection of the upper eyelid by the brow ridge (Fig 4). It often presents as a papule that progresses into a firm lump with pearled edges and central ulceration. However, it can also present in a more insidious manner, with loss of eyelashes being the only indicator of abnormal tissue architecture. These can be tricky to pick up early. If eyelashes are missing, malignancy should be suspected and confirmed by biopsy.

Fig 3. Periocular basal cell carcinoma
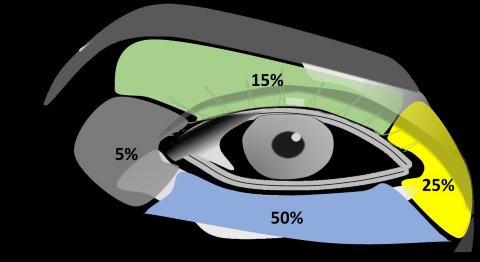
Fig 4. Distribution of periocular skin cancer. Credit Jonathan Norris
Anne
Anne was 70 years old when she presented for a glaucoma assessment. She was fit and well and took no regular medications.
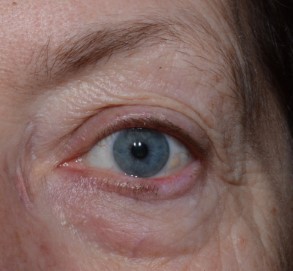
Fig 5. Left lower eyelid infiltrative basal cell carcinoma
This patient was unaware of an eyelid lesion. We can see there was a region of madarosis telangiectasia. The eyelid required a biopsy.
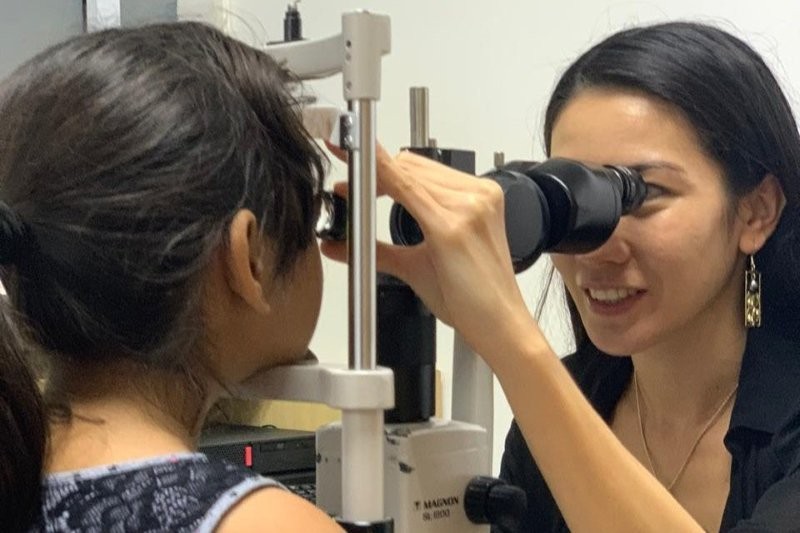
June
June was 48 years old with a four-month history of a left lower eyelid lump (Fig 6). She was prescribed methotrexate for inflammatory bowel disease.
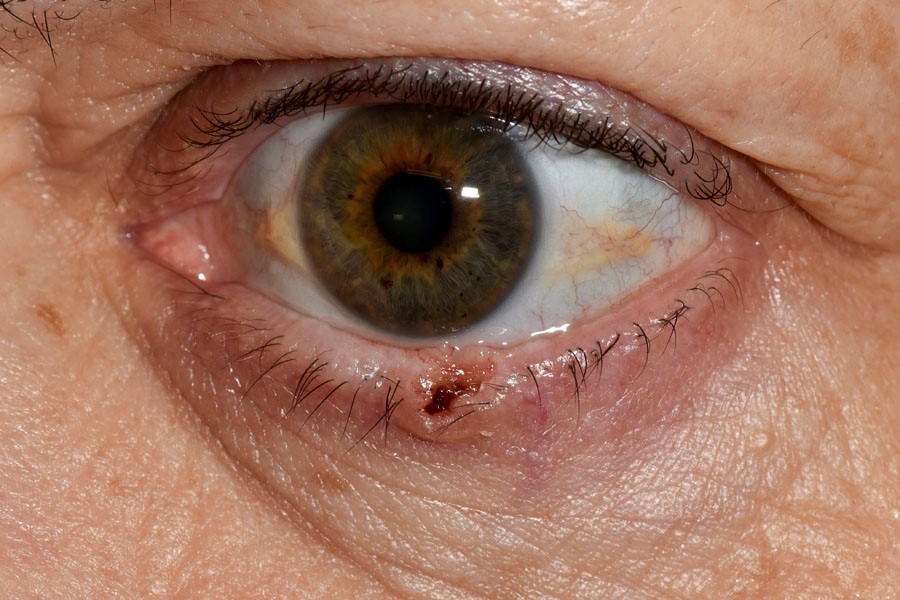
Fig 6. Left lower eyelid nodular basal cell carcinoma
Immunosuppression increases the risk of developing skin cancer and can be present in younger age groups than you would usually expect. This eyelid needs to be referred for a wedge excision/biopsy.
SCC comprises 5-10% of periocular malignancies and can present as erythematous scaly patches, small nodules or ulcerated lesions, again predominantly on the lower eyelid3. Unlike BCC, SCC may be preceded by actinic keratosis – premalignant lesions which are often sandpapery and scaly in texture. It can often be difficult to clinically differentiate BCC and SCC, but if there are malignant features, a biopsy is warranted.
Melanoma makes up only 1% of eyelid cancer; however, the frequency of metastasis and death is high, with a 10-year mortality rate approaching 30%4. As with all melanoma, the depth of invasion is correlated with a worse prognosis.
Prompts for biopsy
If a lesion is suspicious, it requires a biopsy. If the lump is nodular or small this will likely be an excisional biopsy where the entire lesion is removed. If the lesion is poorly circumscribed, not easily visible or large, an incisional biopsy is performed to establish the diagnosis. This will give an indication of how aggressive a tumour may be and how much tissue needs to be removed.
In the eyelid, tissue preservation is key - removal of tumour while conserving as much tissue as possible – to minimise reconstruction requirements and optimise functional and cosmetic outcomes.
In summary, consider referring for biopsy of the lesion if there is:
- A history of growth or bleeding
- Madarosis (loss of eyelashes or brows)
- Central ulceration
- Telangiectatic vessels
- Risk factors such as immunosuppression or history of previous skin cancer
References
- Sun M, Rajak, S, Delva D, Smith H. Periocular basal cell carcinoma: a comprehensive review. Expert Review of Ophthalmology (2017); 12(3);221-232
- Gulleth Y, Goldberg N, Silverman RP, Gastman B. What is the best surgical margin for a BCC: a meta-analysis of the literature. Plastic Reconstructive Surgery (2010); 126:1222-1231
- Limawararut V, Leibovitch, I, Sullivan T, Selva D. Clinical and Experimental Opthalmology (2007)
- Chat F, O’Donnell B, Whitehead K, Ryman W, Sullivan T. Treatment and outcomes of malignant melanoma of the eyelid. Ophthalmology (2007); 114(1):187-92


Dr Liz Insull trained in the UK and New Zealand and is a cataract and oculoplastic surgeon based at Eye Institute Hawke’s Bay. In 2021 she was awarded ‘Trainer of Excellence’ by trainees in RANZCO’s New Zealand network.