Privacy versus AI screening support: Australasia lags behind US
Auckland University’s Dr Ehsan Vaghefi, CEO and co-founder of Toku Eyes, has just launched the company’s second AI retinal screening product, Oraicle, in the US. The company’s technology saves sight and lives by identifying those most at risk of diabetic retinopathy and cardiovascular events. So why is Australasia now lagging behind the US, asked Drew Jones.
How does Oraicle differ from your other AI tool, Theia?
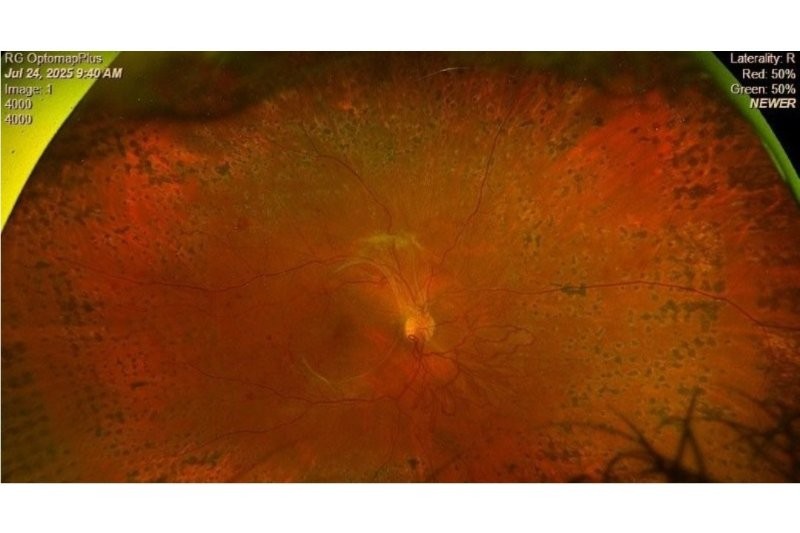
Both artificial intelligence (AI) tools use retinal scans as part of the data input. Theia is about detecting blinding conditions in the eye, such as diabetic retinopathy DR), maculopathy, macular degeneration and glaucoma, whereas Oraicle is about estimating the cardiovascular risk of the individual.
Does the large US population suit your business model?
Yes, on several levels. The cost per person drops when the usage goes up, since the amount of cloud capacity required doesn't scale linearly with the population. And when you capture more data, your AI becomes more accurate. We are not interested in the individual view, we want a population-based view. We can create a pretty accurate map of, for example, cardiovascular risk using Oraicle. Because we're screening a lot of people, we can say which portion of the population has a higher risk, where that risk is and how we can reduce it.
Something we've been working on is feeding the AI data into the informatics platforms we have, which are more about data visualisation and prediction. So AI converts mundane information into data gold. But it’s when you turn data into visual informatics that it becomes really powerful for insurance companies, for healthcare systems, for decision makers. The bulk of the US population is covered by some sort of private insurance, which essentially means as soon as you recruit one of the few large insurance companies, you’ve onboarded a large part of the population, because insurance companies move faster to a ‘yes’ or ‘no’ than the public sector.

Dr Ehasan Vaghefi
How do you envisage the US data being used?
Close to 5% of the US healthcare system consumes about 40% of its resources, because those people that have an end event are the costly ones. So even if you could push that back by a few years, we've saved the insurance company a huge amount of money. At the end of the day, it's always a conversation about efficiencies – dollars saved. So if we can improve someone’s cardiovascular risk, make sure that they don't end up with an event, every insurance company will be interested.
You can quickly build up knowledge on which part of society is suffering more from what, which is really interesting when it comes to targeting resources, running awareness campaigns and education. People tend to think of us as an AI company, but I've started to think of us as a health informatics company that uses AI to mine data.
Are concerns over who owns the data an obstacle to your products being more widely used?
That certainly plays into it, but to me it's a sort of inverted argument. If we are saying ‘let's keep the data private’, which I appreciate, we’re also denying the patient the best care they could have received, because you're limiting the information informing that person’s care.
We were recently talking to one of the largest hospitals in Australia, which is dealing with uncontrolled hypertensive people who are likely to have a cardiac event soon. Our technology could identify who needs priority care, because a hospital has to prioritise. But we came to a roadblock – “We cannot give you our data.” So their idea was to physically install our tech in the hospital. But, firstly, our technology is so computationally heavy that they would need a supercomputer, which would be so expensive it would defeat the purpose. Secondly, if I bring my system into the hospital, there has to be a firewall, so I don't have access to it and I can’t maintain or update it.
So they misunderstood the model?
Absolutely. I think because of bad experiences about patients’ records being leaked, governments have become too sensitive about patient information. I appreciate that, but not sharing information leads to worse outcomes. The more I know about you, the better care I can provide.
Are you lobbying local governments to adopt the tech more widely?
Both products are registered with New Zealand’s Medicines and Medical Devices Safety Authority (MedSafe) and are commercially available here. Theia is being used in a few regions in New Zealand, as well as in 70 clinics across India. We see India as the largest market for Theia, due to the sheer demand for diabetic screening and lack of retinal specialists.
Governments here are not incentivised necessarily by dollars saved – it's more about policies and appealing to the public. We’re trialling Theia and Oraicle in Australia and New Zealand. We have a few customers paying small amounts to use these technologies, but the major rollout over here depends on the government or main health insurer.
In Australia the problem is a bit more recognised than in New Zealand. Unfortunately, Australians are dying because the health system cannot prioritise. Every hospital is a silo, which I just don't understand. We’re trying to be one of the voices to change that. At least in New Zealand the data is meant to be shared between DHBs (regions).
Will the new Health NZ model better suit your tech?
I certainly hope so. The devil is in the details, but I’m happy with the idea of Health NZ because the more centralised a system is, the better care it provides.
Healthcare should not be a postcode lottery. Your care provider should have access to all the information about you and people like you – what worked and what didn't in, say, 100 similar cases. But if you have been receiving treatment somewhere else, even in a different part of the country, and your doctor doesn't see it, that’s no good. Or if yours is a special case and there have been fewer than 100 similar cases that are not on public record, it probably means your doctor is not going to treat it as unusual – they will try to fit it with the cases they know of.
In Australia and New Zealand, we're just going to keep working at it. It's slower progress, but when we show how we’re making a difference in the US, hopefully that will be noticed here.
For more, see https://www.nzoptics.co.nz/articles/archive/what-makes-good-healthcare-ai/ and https://www.nzoptics.co.nz/articles/archive/top-scores-for-kiwi-ai-screening-tool/