The four-year diagnosis – a cautionary tale
A recent case illustrates that, despite recent advances in the diagnosis and management of dry eye disease (DED), its identification often remains elusive. To prevent misdiagnosis, clinicians are reminded to watch out for key features.
Case report
Mr A: a 65-year-old male, attending oculoplastics clinic for seventh time in four years with ongoing watering eyes; re-referred to recheck his tear ducts.
- Syringing at first presentation – patent; no help with watering
- Punctal plugs – left in for a few weeks to dilate puncta; no perceived benefit
- Three-snip punctoplasty – no perceived benefit
- Maxitrol – helped a little while using it, would like it again
- Vita-Pos – used as recommended; no perceived benefit
On questioning:
- Intermittent bilateral watering
- Hyperaemia
- Feels “like salt in my eyes”
- Eyes water in the wind and after using computer
On examination:
- Normal lid position, normal tear meniscus
- Patent puncta
- Clear cornea, quiet conjunctiva
Aetiology of epiphora
Almost everybody experiences watery eyes in the cold or wind – the eye protects itself by watering. While epiphora in adults is a mostly nonspecific finding, its aetiology can be classified as reflex tearing, reduced tear outflow, or lacrimal hypersecretion, each with numerous causative or contributing factors. Primary hypersecretion of the lacrimal gland, as well as drainage insufficiency, are relatively rare; the latter often being clinically evident and thus easily ruled out. Bilateral intermittent watering, which can be asymmetric, can occur with or without discomfort, but almost never relates to tear duct blockage. Once structural, mechanistic impediments have been ruled out, it’s critical to consider the structure of tears.
Tears and dry eyes
Tear overproduction offers the ocular surface protection from hyperosmolar stress secondary to tear film hyper-evaporation, secondary to a deficiency in the quality and/or quantity of meibum – a hallmark of dry eye disease. Some patients are more symptomatic than others, with many environmental and lifestyle factors contributing. Computer work, for instance, decreases both blink rate and completeness, adding to evaporative stress. A concurrent itch usually points to an allergic component.
In light of the common misconception that ‘dry eye’ means lacrimal insufficiency, it’s worth reiterating that dry eye exists on a spectrum between aqueous and evaporative deficiency. Most often it is the latter, and quite often it involves both, with tear film instability being a universal marker.
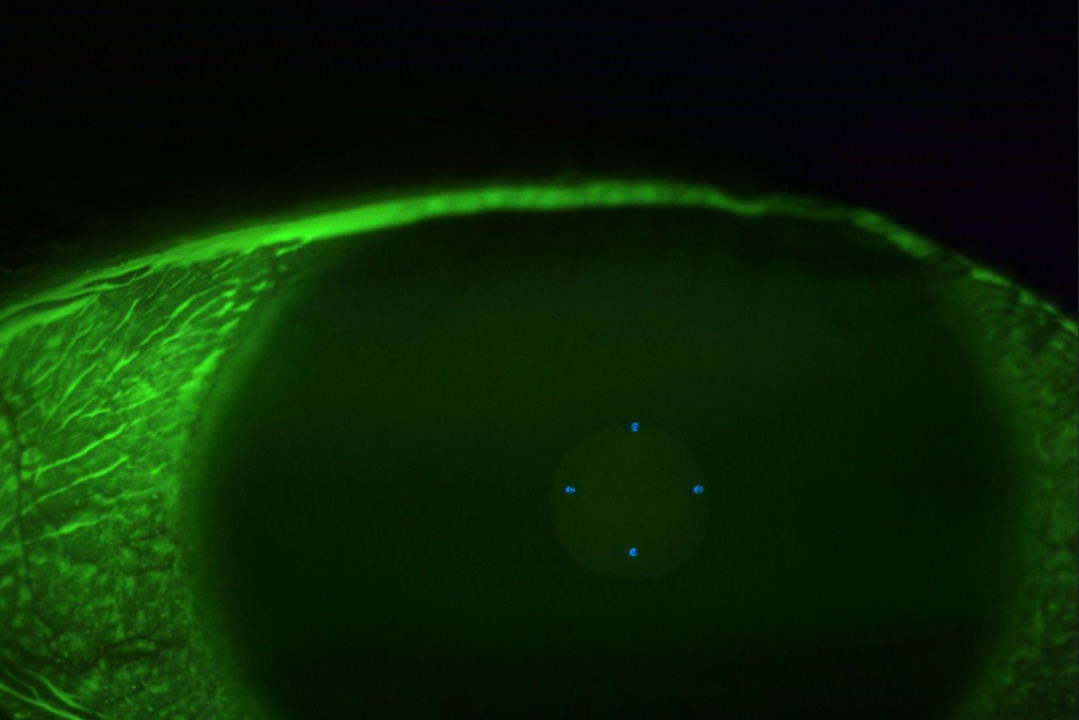
Tear hyperosmolarity – increased saltiness of the tears – another central marker for DED, is often accompanied by an inflammatory response, translating into symptoms of irritation for the patient, described in this case as “like having salt in the eyes”. Osmolarity measurement would thus be useful, where available, as would a non-invasive measure of tear film breakup time, and meibography.
Management
Tear duct obstruction is typically painless and unilateral. Unless an obvious cause for epiphora and discomfort, such as lid malposition or trichiasis, is noted, it is best to start with the least invasive intervention. This most often means managing the ocular surface and tear film instability in the first instance – and steroids should not be the first consideration! Although steroids can swiftly reduce inflammation and drastically improve comfort, they are no long-term solution, as they do little to address the root causes of hyperosmolarity or tear film instability. When long-term anti-inflammatory is required, a steroid-sparing agent, such as cyclosporin 0.1% or tacrolimus 0.1%, can be a highly effective and safer alternative.
In this case, azithromycin (500mg OD PO for two days) or doxycycline (50mg OD PO for 3/12) are better first-line anti-matrix metalloproteinase protein agents to reduce inflammation by decreasing lipases. However, these do little to address the stagnant oil in the meibomian glands, and need to be combined with heating and physical expression of meibomian gland oils. With obstructive meibomian gland dysfunction being the leading cause of DED, the treatment of choice should primarily involve the application of heat and physical expression, such as warm compresses and lid massage, intense pulsed light (IPL), or thermal pulsation, for example.
Topical lubricants are a great supportive, if not often necessary, addition. Adding more aqueous to an already watering eye may seem like a waste of time, but lubricants can ease discomfort in the shorter term and research, published by the University of Auckland’s OSL team as part of an international collaboration, confirms they can help restore tear film homeostasis, breaking the vicious circle of dry eye disease in daily, frequent use (minimum four times daily). To avoid washing away the lipid layer, opt for a good quality, lipid-based formulation.
Better oil production can be encouraged with azithromycin (see related story p40), oral omega-3 and with IPL, but it is vital to express to remove the old oil – no existing drops, ointments or tablets are effective in expressing the stagnant oil. That requires heat applied at 42⁰ for 10 minutes followed by lid margin massage. A microwavable wheat bag is effective at retaining the heat for this duration, unlike a hot flannel, but patients need to be reminded that this takes a few weeks of daily attention to slowly increase tear film robustness.
Vita-Pos contains retinoid, a compound used therapeutically to reduce oil gland function in acne and cosmetically as retinol cream, which causes the skin to dry and sometimes peel, with dry eye a common side effect, warranting cautious use. Allergies can further destabilise the tear film and are managed with olopatadine or tacrolimus.
Summary
In this case,an early recommendation for heat and gland-expression-based management of tear film instability may have saved the patient multiple visits to the eye clinic, a punctoplasty and the disappointment of ineffective treatments!
It’s important to manage the ocular surface in all cases of epiphora and investigate the tear drainage system only when epiphora is ongoing, usually unilateral and not associated with discomfort (as this is when issues such as drainage insufficiency due to lid malposition, nasolacrimal duct obstruction or punctal occlusion can be suspected) or where there is obvious mucocoele or dacryocystitis. If there is discomfort, bilateral or intermittent watering, presume evaporative dry eye to be the most likely cause of epiphora before investigating the tear drainage system.
Patients with nasolacrimal duct obstruction who do not wish to proceed with a dacryocystorhinostomy can also manage any tear film instability with heat and lid massage, which may reduce watering to a tolerable level. Remember, punctal plugs for aqueous deficiency is a recognised strategy, so blockage in the tear drainage system for certain patients may actually work in their favour and is not by itself a reason for surgical intervention.

Dr Simon Dean is an ophthalmologist specialising in oculoplastics at Manukau Super Clinic in South Auckland, New Zealand.