Workshopping gonio and foreign bodies
The 2018 Eye Institute Annual Conference once again kicked off with two very practical workshops, this year tackling foreign body removal and gonioscopy.
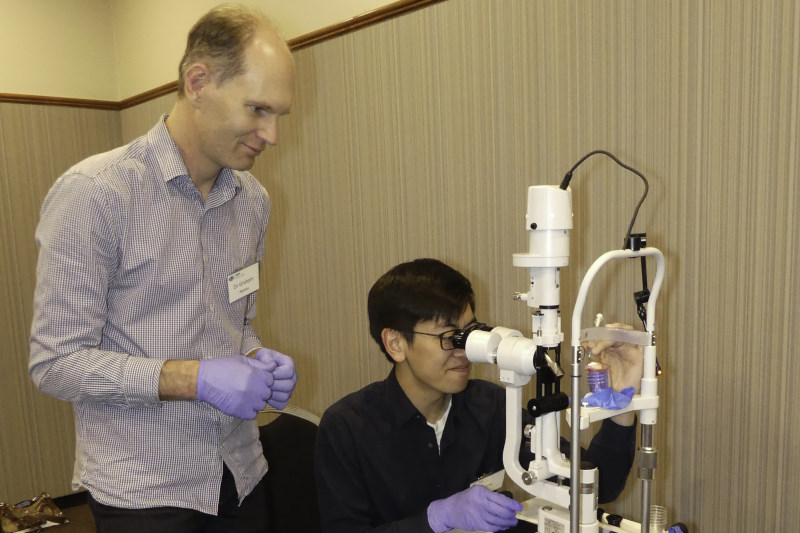
Corneal foreign body removal
Dr Shanu Subbiah introduced the foreign body removal workshop with an overview of how foreign bodies tend to enter the eye and stressing the importance of taking a thorough history of the patient’s work and hobby practices to provide insight into whether there’s likely to be a foreign body in their eye, what it might be and thus how bad it could be. In summary, high velocity particles can cause globe penetration, metallic bodies cause rust rings, there’s a risk of fungal infection with vegetative bodies, and foreign bodies don’t cause recurrent erosion syndrome.
Foreign bodies tend to be ACC cases and may also have a legal element to them too, so meticulous documentation is important, he said. In general, always irrigate, check visual acuity, pupil response and if there are any signs of penetration. Foreign bodies on the conjunctiva can be removed with a sterile cotton bud, while other corneal foreign bodies may need to be removed with a sterile needle or other sterile instrument. Use adequate topical anaesthetic (benoxinate 0.4% or amethocain 0.5% or 1%); ensure you use the needle tangentially to reduce the risk of corneal penetration and use a burr for rust removal two to three days after removing the primary metallic foreign body. Dr Subbiah also suggested using a larger needle to get underneath the foreign body, so using it more as a pallet, to prise it out of the cornea. Given the epithelium has been broken, there’s always a risk of infection with foreign body removal so prescribing antibiotics is standard. Overall, optometrists should only do as much as they feel comfortable doing and if they are concerned they should refer, he said.
Participants then got to grips with practising their own foreign body removal techniques using pigs’ eyes, carefully penetrated with foreign bodies by the workshop’s co-host Dr Graham Reeves.
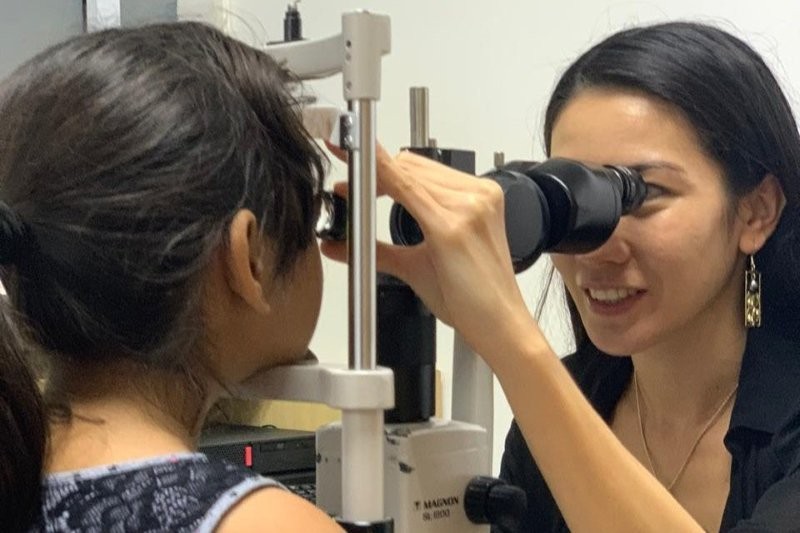
Gonioscopy
Drs Jay Meyer and Divya Perumal ran the second workshop which provided attendees with a very hands-on look at the practical dos and don’ts of gonioscopy.
Key to conducting a successful gonioscopy is ABCD, said Dr Perumal: A for the local anaesthesia amethocaine (tetracaine); B for black-out, making your room as dark as possible; C for corneal wedge, or parallelopiped, a technique for identifying the anterior border of the trabecular meshwork, especially useful in patients where the border is difficult to see; and D for dynamic gonioscopy (compression or indentation gonioscopy), where gentle pressure is placed on the cornea to aid diagnosis. As to grading, Dr Perumal says normally a good description is enough for a referral from an optometrist, though if the referral goes the other way then ophthalmologists tend to use a grading scale.
For those wanting more detail, Dr Perumal recommended Gonioscopy: A Text and Atlas (with Goniovideos) 1st Edition, by Tanuj Dada.
Equipment for the foreign body and gonioscopy workshops was kindly provided by OptiMed and the Ophthalmic Instrument Company (OIC) respectively.