CLs in albinism – BLENNZ’s akonga experience
A group of researchers associated with the Blind and Vision Education Network of New Zealand (BLENNZ), including myself, Dr Shuan Dai and Hadyn Treanor, undertook a study to assess the visual benefits of tinted and clear contact lenses (CLs) in akonga (students) with albinism. The aim was to assess the clinical visual impact of the optical corrections and the functional experience of those who participated to better understand what was important in their everyday lives.
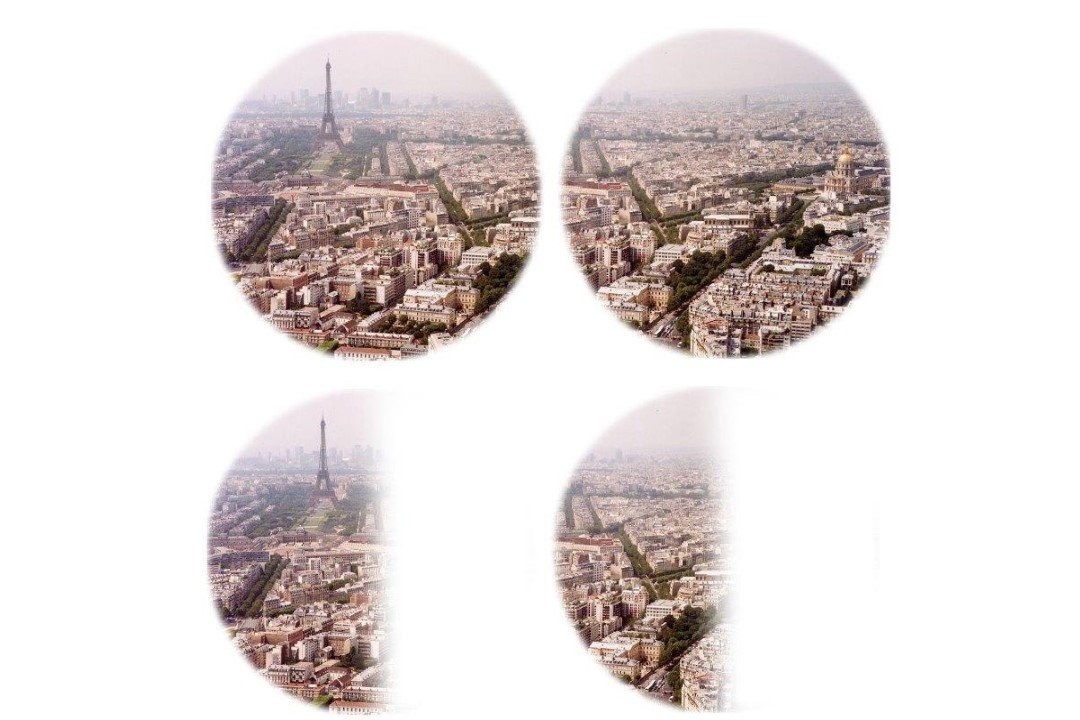
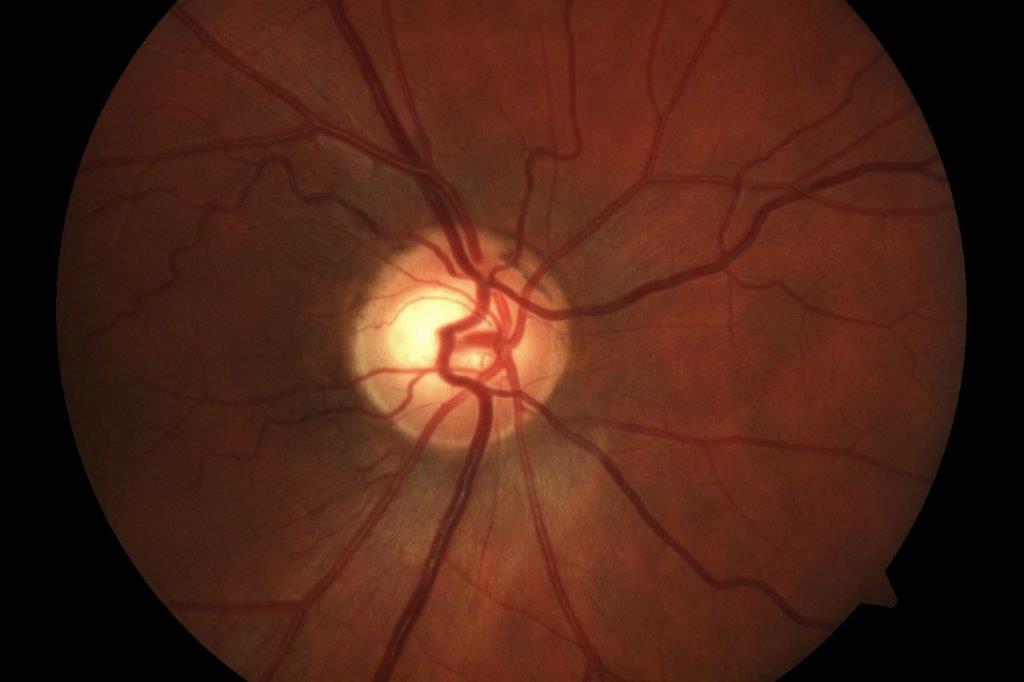
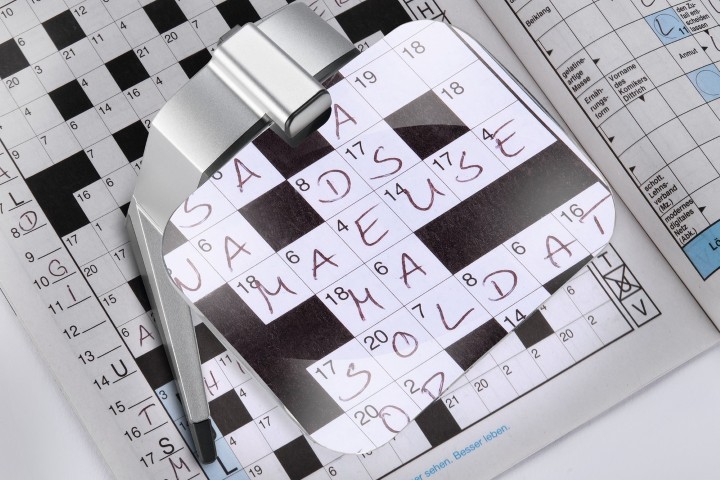
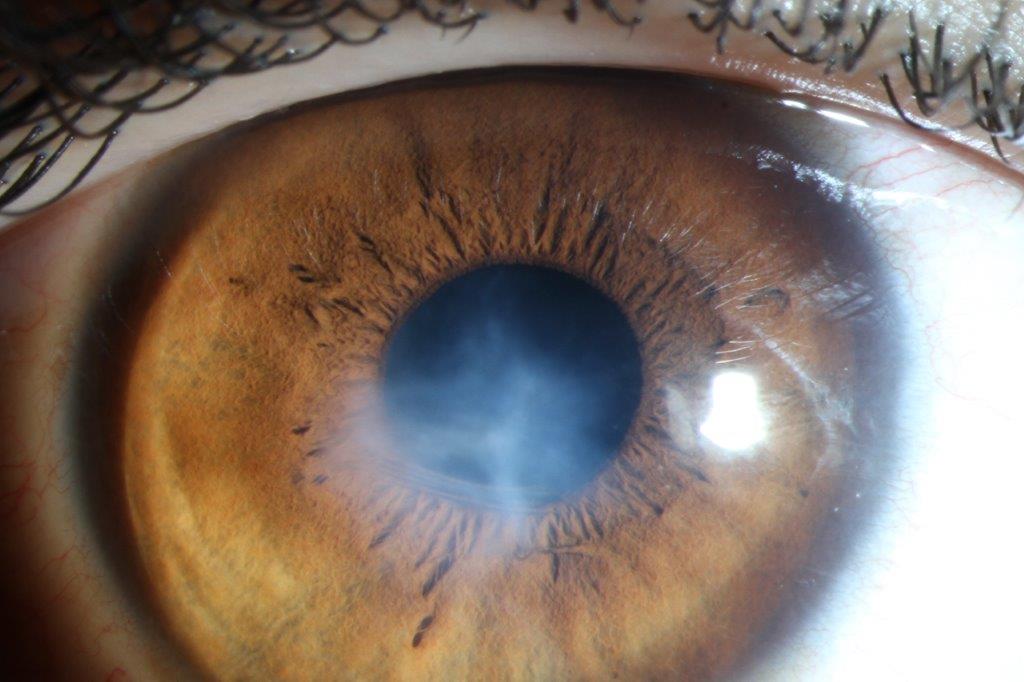
Albinism is an inherited disorder impacting the melanin production pathway, resulting in reduced pigmentation of the hair, eyes and skin or, in cases of ocular albinism, the eyes alone. Children with albinism have visual impairment due to a combination of nystagmus, foveal hypoplasia, iris transillumination and high refractive errors (Figs 1 and 2).
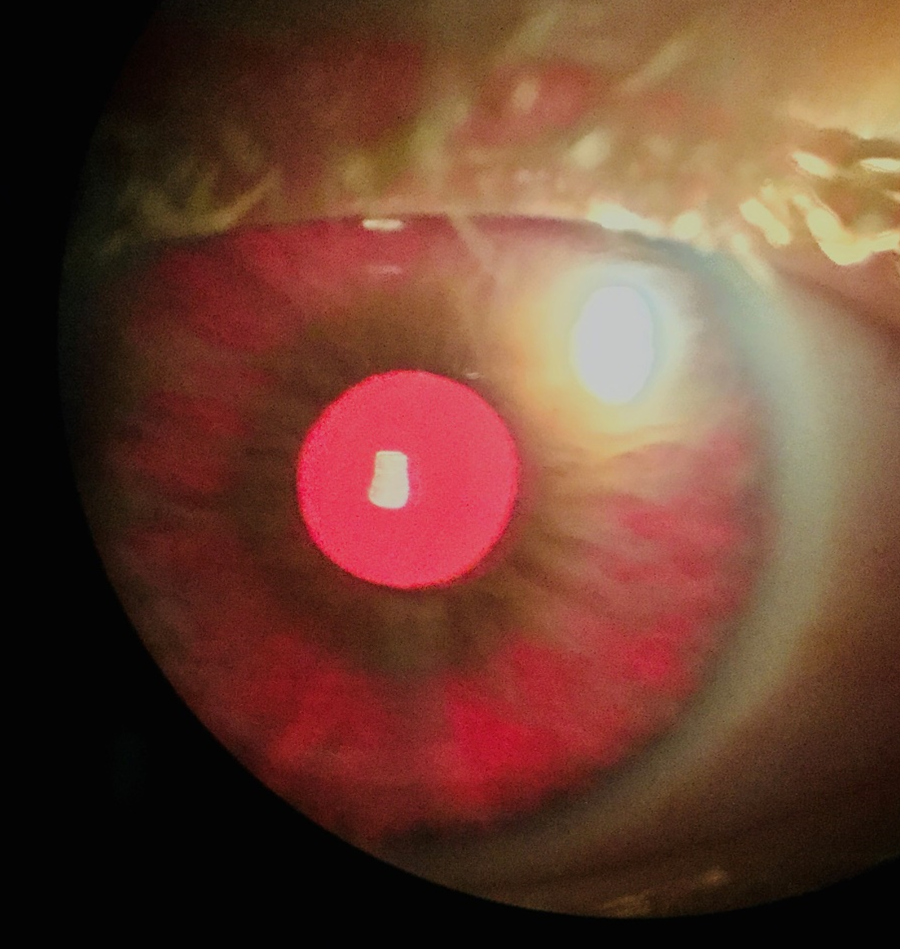
Fig 1. Transillumination in an eye with oculocutaneous albinism.
Note the diffuse transilluination and spoke-like pattern. Some blur
is present due to this individual’s high rate of nystagmus.
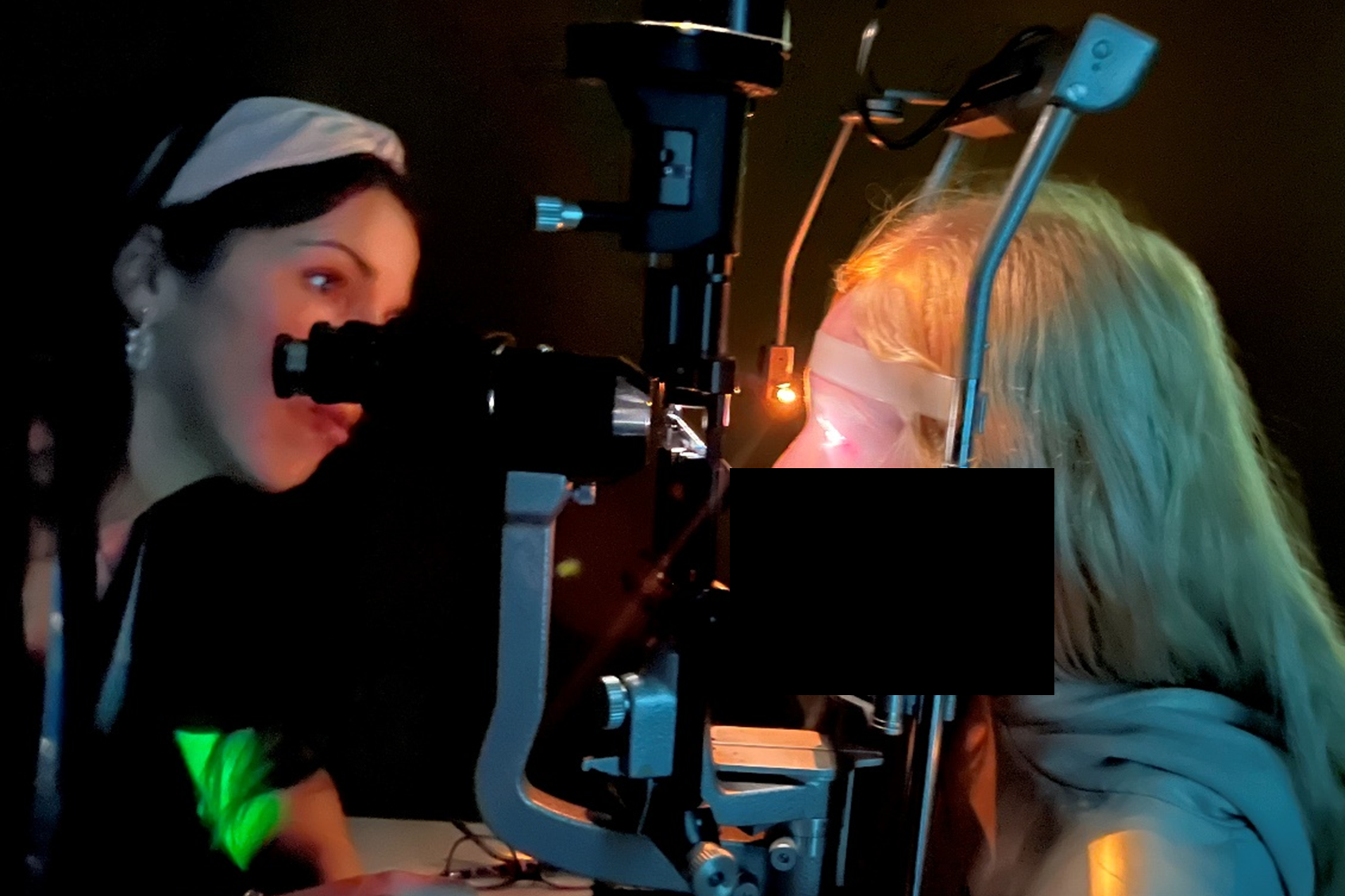
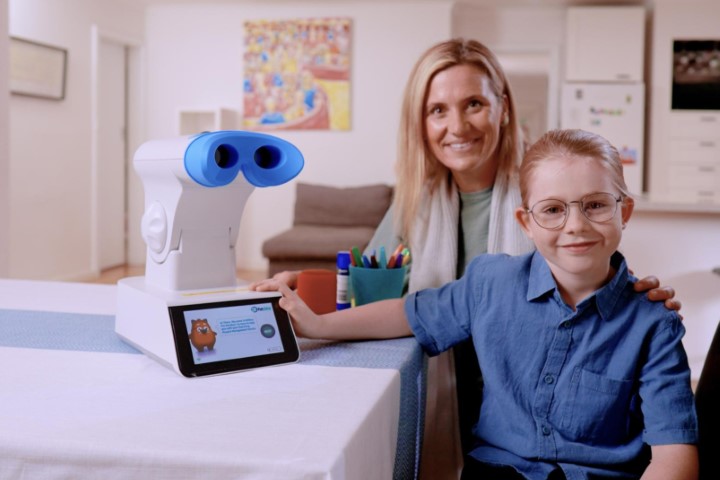
Fig 2. Dr Sam Simkin makes a slit-lamp assessment of a student
with oculocutaneous albinism
Prescription of glasses for individuals with albinism is variable, even with refractive errors, due to the changeable visual improvement achieved. Many children with albinism report that their glasses are not useful, possibly due to glasses exaggerating the impact of the nystagmus behind the fixed lens causing visual discomfort. The use of tinted lenses or an artificial iris may reduce glare and photophobia in patients with albinism1,2. In some case reports, the reduction of ocular stray light in this way also resulted in improved objective visual acuity (VA) measurements3.
Tinted contact lenses with a small aperture clear pupil, designed to work like an artificial iris, have been suggested for cosmesis (and have been used as such since the 1950s3,8) and improving nystagmus4. The proposed mechanisms for improved vision through CLs compared with glasses are:
- Increased time viewing through the correct visual axis5
- Possible improvement in nystagmus through additional vergence and accommodative effort with CLs4-6
- The similarity to an artificial iris to reduce glare, photophobia, VA and nystagmus intensity1,2,7,9
Method
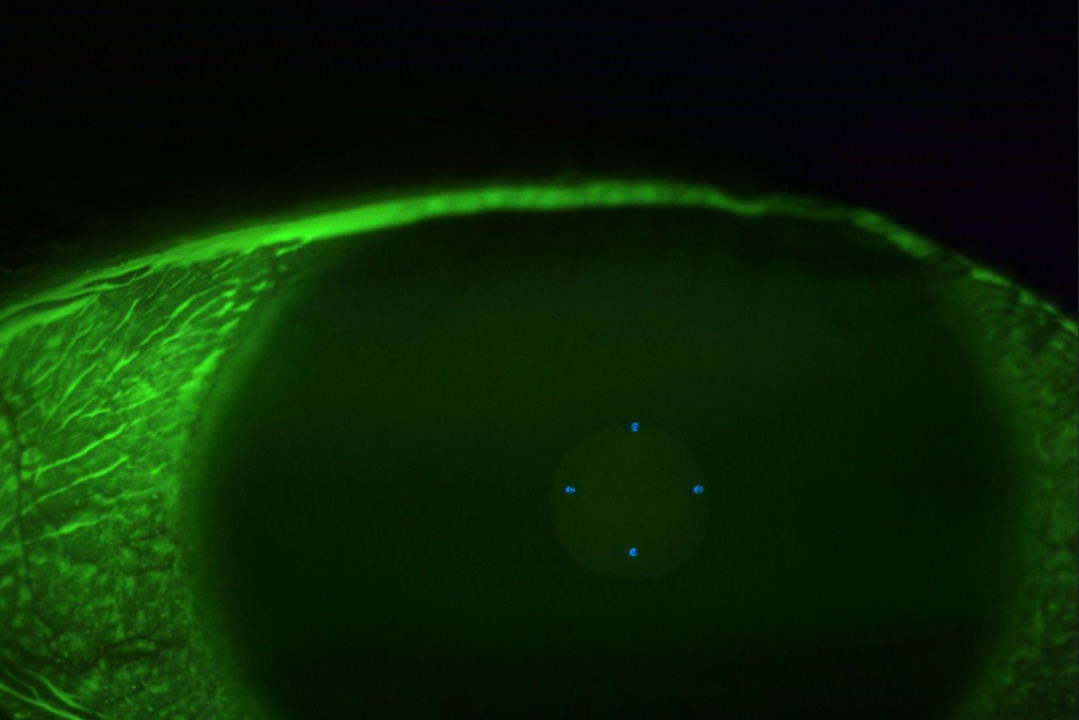
We assessed both clear and tinted contact lenses with a clear central aperture (Fig 3) for both objective and subjective visual impact when compared to glasses. NuToric (Capricornia) custom CLs were used, in both clear then tinted, with a 90% opaque tinted ‘iris’ with a 3mm central clear pupil to mimic a photopic pupil size, similar to other reported cases. The goal was glare reduction equivalent to an eye without transillumination.

Fig 3. Tinted contact lenses with clear central apertures,
as used in this study
Ethics approval was provided by the Health and Disability Ethics Committee and the BLENNZ board of trustees. Recruitment for the study began in January 2020, which coincided with the Covid-19 pandemic and subsequent lockdowns, impacting both recruitment and follow-ups. However, a total of 13 participants were able to complete the full protocol. The demographics and VA of those recruited were not statistically significantly different from the full cohort of individuals with albinism enrolled at BLENNZ. Questionnaires were used throughout to understand the akonga experience alongside clinical assessment of vision.
The right eye results were used only for analysis. Glasses correction had a mean spherical power of +2.78DS (range -19.75 to +10.50DS), with astigmatism correction of -1.73DC (range of -3.75 to 0.00DC). This aligned with expected high prescriptions of hyperopia, myopia and astigmatism, all known to be present in individuals with albinism. Questionnaires indicated 50% of akonga wore glasses reliably, 26.7% did not wear glasses (even though they were prescribed) and 23.3% were variable wearers who stated they used them primarily for glare reduction via tint or photochromic lenses. As expected, higher refractions were associated with increased likelihood for glasses wear. The CLs fitted had a diameter of 14.5mm with base curves ranging from 8.2-8.8mm with 8.4mm being the most common. There were no significantly different prescriptions between glasses and CLs prescribed once vertex distance was accounted for. CL fitting was achieved through trial fittings due to nystagmus making topographical assessment of corneal curvature unreliable. Akonga got the opportunity to trial both tinted and clear CLs, which were supplied in a randomised manner with a minimum six-week trial of each.
Results
There was no significant difference in VA between the optical correction options trialled. Clear CLs were the most preferred option, closely followed by glasses, although there was an interest in tinted CLs without the central clear aperture from a large portion of the participating group. This may be due to the interference of the edge of the aperture coming into the field of view with lens movement.
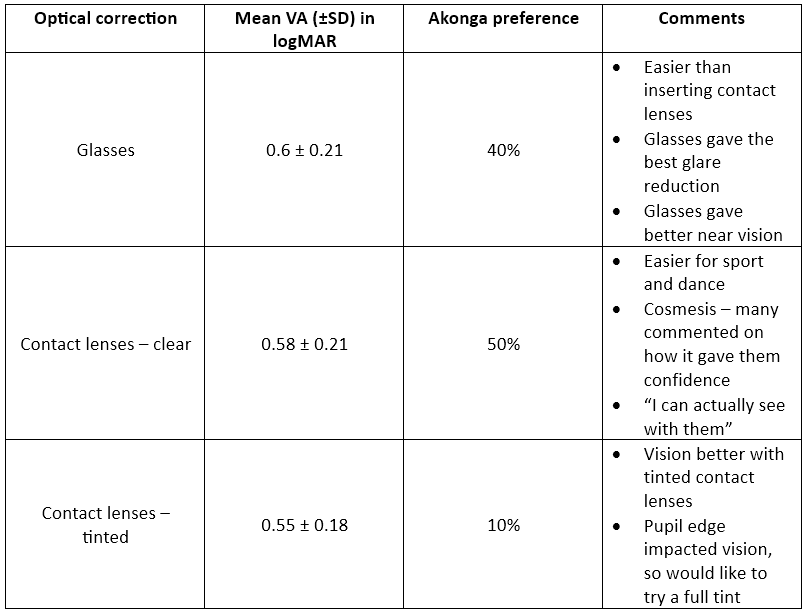
Table 1. Visual acuity, akonga preference and specific feedback comments on the optical correction options trialled
Discussion
Fitting contact lenses in this group was challenging due to their low vision, young age and nystagmus and, unfortunately, our study was limited by small patient numbers and restricted follow-up due to Covid-19. We were not able to determine the CLs’ impact on nystagmus or any statistically significant objective visual differences; however, the study still provided some interesting insights for clinical practice.
When considering optical options, even if glasses are not being used, contact lenses should be discussed, since glasses wear is not a reliable indicator of CL benefit in this group. Tinting options for glasses and CLs should be a key consideration in individuals with albinism; unique combinations such as clear contact lenses with plano tinted glasses may provide the best solution. It is important to work closely with akonga and whānau to maximise visual comfort and function. Since clinical measurements may not provide the answer for the best visual correction in individuals with albinism, patients’ visual experience should be at the forefront of our minds, with trials of a number of options potentially needed to find the best visual support.
This project was generously funded by the Middlemore Foundation.
For further discussion of BLENNZ’ work with individuals with albinism and optical correction, feel free to contact me at samantha.simkin@blennz.school.nz.
References
- Schwering M, Kumar N, Bohrmann D, et al. Refractive errors, visual impairment, and the use of low-vision devices in albinism in malawi. Graefes Arch Clin Exp Ophthalmol. 2015;253(4):655-661.
- Karabas L, Esen F, Celiker H, et al. Decreased subfoveal choroidal thickness and failure of emmetropisation in patients with oculocutaneous albinism. Br J Ophthalmol. 2014;98(8):1087-1090.
- Phillips A. A prosthetic contact lens in the treatment of ocular manifestations of albinism. Clin Exp Optom. 1989;72(2):32-34.
- Vincent Stephen J. The use of contact lenses in low vision rehabilitation: Optical and therapeutic applications. Clin Exp Optom. 2017;100(5):513-521.
- Liu S, Kuht H, Moon E, Maconachie G, Thomas M. Current and emerging treatments for albinism. Surv Ophthal. 2021 Mar 1;66(2):362-77.
- Jayaramachandran P, Proudlock F, Odedra N, Gottlob I, McLean R. A randomized controlled trial comparing soft contact lens and rigid gas-permeable lens wearing in infantile nystagmus. J Ophthalmol. 2014;121(9):1827-1836.
- Saeed F, Schlange D, Najafi T. Sustained benefits of therapeutic tinted contact lenses in patients with albinism. Invest. Ophthalmol. Vis. Sci. 2013;54(15):2778.
- Vincent Stephen J. The use of contact lenses in low vision rehabilitation: Optical and therapeutic applications. Clin Exp Optom. 2017;100(5):513-521.
- Omar R, Idris S, Meng C, Knight V. Management of visual disturbances in albinism: a case report. J Med Case Rep. 2012;6:316

Dr Samantha Simkin is a therapeutically qualified optometrist with a PhD in childhood visual impairment. She has multiple peer-reviewed publications and regularly speaks at conferences on paediatric optometry, myopia management, causes of visual impairment and management of low vision in children. Following parental leave, she will return to BLENNZ research and clinical work with Judd Opticians and Te Whatu Ora Taranaki.