Dry eye technology: improving outcomes
My practice focuses on specialty eye care and, much to my surprise, dry eye continues to be one of our main drawcards and is continuing to grow. A lot of the success we have experienced with dry eye has been due to the implementation of the latest dry eye technology. From a diagnostic perspective, dedicated systems provide a level of detail that allows for more precise diagnosis and better monitoring of treatment outcomes; while from a treatment perspective, advanced technology allows for more intense therapy that offers shorter treatment times with improved patient compliance.
Treating dry eye doesn’t happen overnight. It is more of a rehabilitation process than expecting results from a quick, one-off treatment. It also requires patient buy-in and trust in your diagnosis and treatment plan, and this trust needs to endure for months as the treatment progresses, often with only subtle improvements in symptoms in the initial stages. Key to keeping that trust intact is the use of technology.
Meibography: a game changer
One of the key developments in dry eye diagnostic technology has been the ability to image the meibomian glands. Meibography allows you to visualise how blocked (damaged) the glands are and judge how quickly you might expect your treatment to work. More importantly though, it allows the patient to see their meibomian gland dysfunction (MGD) for themselves. This has a powerful effect on patients and sets the foundation for good treatment compliance going forward.
Imaging and encouragement
While imaging is a powerful tool, so too is encouragement. Combine the two together and you have a recipe for good compliance. Even in the absence of symptom improvement, when patients see their clinical signs improving, confirming their hard work is paying off, it encourages them to persist with their treatments. A dry eye topographer, that allows you to demonstrate improvements in lipid layer thickness and non-invasive tear breakup time, is key to reassuring patients that their symptoms are likely to improve soon and encourage them to follow through with your treatment recommendations.
A dry eye topographer also allows you to accurately monitor treatment progression and share the results. Some treatments become effective over an extended period, but without technology to confirm subtle changes in the tear film or ocular surface, it can be difficult to convince a patient to continue with current treatments without obvious symptomatic improvement, and this could force you to alter a treatment strategy that might have been very effective if given sufficient time.
A patient of mine who went from depending on autologous serum drops to requiring no drops at all, recently told me our follow-up sessions were key to encouraging her to continue with treatment. Seeing improvements in measurements gives patients reassurance they are not wasting their time.
Technology for treatment
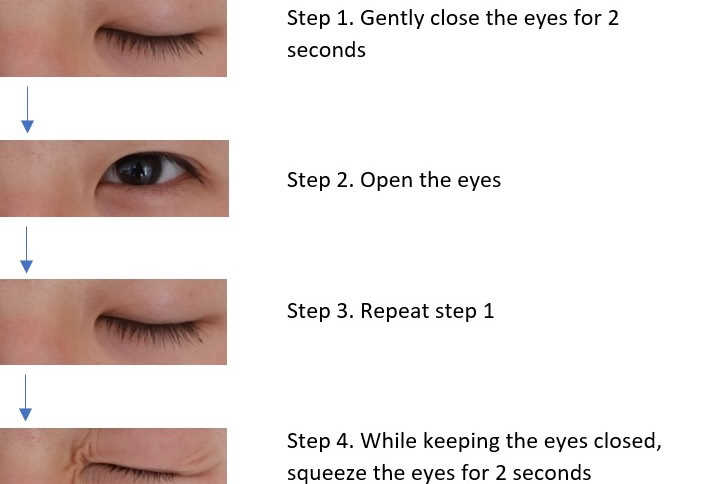
Warm compresses used properly are very effective and I prescribe them routinely. However, for many of my more severe patients, compresses are just not enough to get their dry eye under control. At my practice, I have an extensive range of dry eye treatment options including Lipiflow, and E>Eye intense pulsed light (IPL) and, most recently, I’ve introduced the Rexon-eye.
- Lipiflow
Lipiflow is a great treatment for MGD. It involves a single, 12-minute session of thermal pulsation on the eyelids and symptom improvement is typically noticed after about four weeks. Long-term studies show improvements in signs for up to three years and symptoms for up to two years. I have found that one year is the average, but patients can extend this further if they continue maintenance therapy at home. Longer-term follow-up studies are one of the key advantages that Lipiflow has over other devices as I can confidently give patients an estimate of how long they can expect the effect of their treatment to last. Also, the fact that it requires only one session, makes it a good option for patients that live far away and find it difficult to come in for multiple treatment sessions. I have treated several patients that live outside Auckland and even patients who live overseas. But for patients with very severe gland loss, I tend to go with one of the other treatment options, as I find that the response to Lipiflow is less effective in these patients.
- E>Eye IPL
The E>Eye intense regulated pulsed light or IPL course of treatment involves four IPL sessions spread over a 70-day period. I also add manual expression of the lids after each session. I have found a noticeable improvement with this treatment in reducing lid margin inflammation, therefore I tend to favour this treatment when lid margin inflammation is very visible. I also tend to favour it when meibography shows extensive gland loss, since it is postulated that IPL doesn’t just work on the glands, but also has anti-inflammatory and anti-bacterial effects.
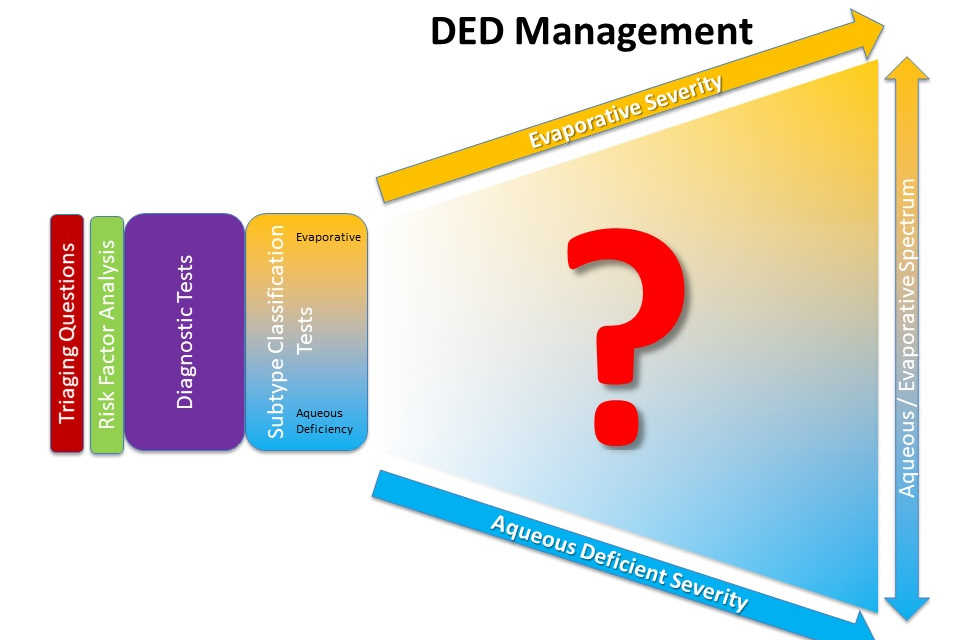
- Rexon-Eye: finally, a treatment for aqueous deficiency
Earlier this year, we became the first practice in New Zealand to acquire a Rexon-Eye device*. I was attracted to the device as early studies showed it resulted in improvements in meibomian gland expression, corneal surface staining and, most impressively, tear secretion. For me, this was the missing tool in our arsenal as we didn’t have a convincing treatment for aqueous deficient dry eye. The treatment uses electrical currents at a therapeutic frequency, termed ‘quantum magnetic resonance’ by the manufacturer, which are applied to the eyelids via goggles. The treatment consists of four, 20-minute sessions over four weeks. Having had the treatment myself, I would describe it as comparable to having a warm compress applied to the eyes.

Ryan Mahmoud treating a dry eye patient with Rexon-Eye
My experience with patients so far has been that it does indeed appear to increase tear secretion and lead to improvements in meibomian gland function. One of its key advantages, is that I find it improves symptoms within one day of the first treatment session. I can therefore test it out on patients before making a decision about proceeding with the remaining three sessions. I have been using it for patients with signs of aqueous deficiency and as a follow-up treatment to Lipiflow when patients want to experience faster results.
In summary, dry eye technology has allowed me to diagnose dry eye better and treat it more effectively. I have been able to achieve favourable results for my patients and offer them relief from their pain and discomfort and, in the end, that’s what this is all about. *
*https://eyeonoptics.co.nz/articles/archive/new-dry-eye-device-unveiled-in-nz/
Ryan Mahmoud is a therapeutically trained optometrist and owner of NVision Eyecare in Auckland, New Zealand. NVision offers speciality services in myopia control, RGP contact lens fitting and dry eye.