How does Covid-19 affect the eye?
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, Covid-19) was declared a worldwide pandemic in 2020, with 750 million cases to-date. A plethora of ocular diseases have been found to be associated with Covid-19, affecting approximately 11% of patients1. As non-hospitalised patients with active Covid-19 infection are often triaged in the virtual setting, it is critical for primary care physicians, optometrists and ophthalmologists to be aware of red flags warranting urgent review.
Here, we discuss our experience with Covid-19 at Auckland Greenlane Clinical Centre and a comprehensive review of the 438 published articles examining ocular manifestations of the virus.
Conjunctivitis
Conjunctivitis and ocular surface disease are the earliest and most commonly reported ocular manifestations of Covid-19 infection, often occurring simultaneously with respiratory symptoms2. Studies have shown that ocular fluids may be a vector for disease transmission, an important reminder that full personal protective equipment, including ocular protection, must be used during examination2.
Scleritis and uveitis
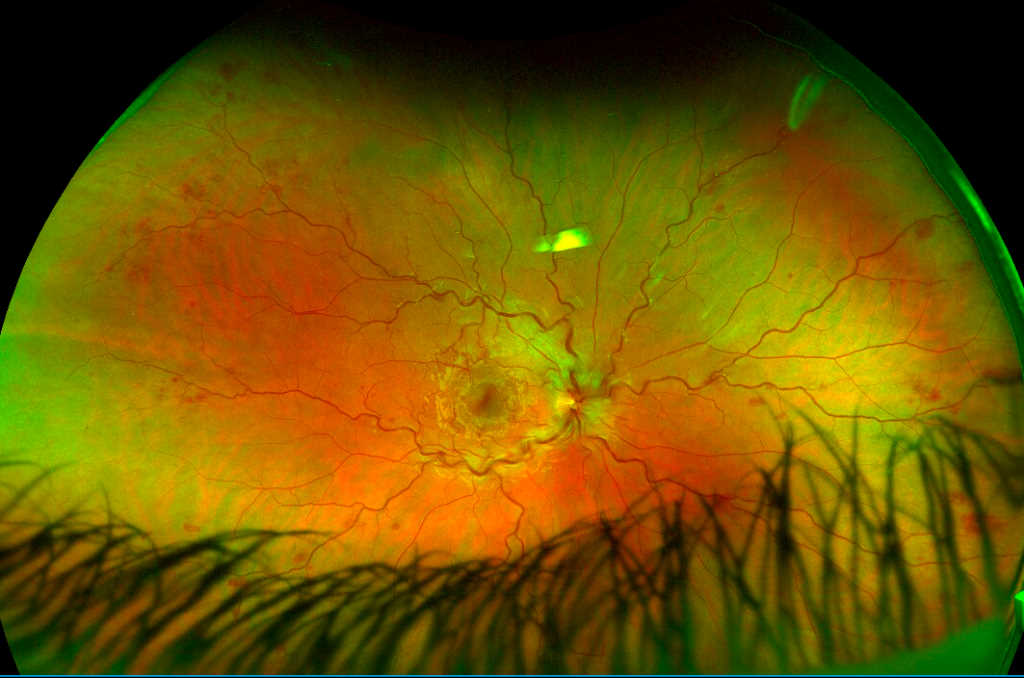
While conjunctivitis is the most common cause for an acute red eye following Covid-19 infection2, the virus can manifest in many structures of the eye. It is therefore important for clinicians to consider other symptoms such as pain, decreased visual acuity or photophobia which may suggest an alternative diagnosis. There have been four cases of Covid-19-related scleritis reported in the literature, the most recent of which was in New Zealand by Wilkinson et al (2023), reporting an otherwise healthy, vaccinated 24-year-old man with bilateral anterior necrotising scleritis3 (Fig 1). Twenty-four papers reported uveitis including anterior, intermediate, posterior and panuveitis, including nine describing healthy children or adolescents who developed anterior and intermediate uveitis as part of a paediatric inflammatory multi-system syndrome. A case series of seven patients reported anterior uveitis with granulomatous signs4. White-dot syndromes, including multiple evanescent white-dot syndrome (MEWDS) (Fig 2), acute macular neuroretinopathy (AMN) (Figs 3-4) and acute posterior multifocal placoid pigment epitheliopathy (APMPPE) have also been described in several cases of Covid-19 infection and post vaccination5,6. While the mechanism is not fully understood, it is postulated that the virus damages capillary endothelial cells leading to hypoxia and microthrombosis, which is thought to impair retinal pigment epithelium cell-barrier function6. Peripheral ulcerative keratitis was also reported in a single patient with rheumatoid arthritis with simultaneous Covid-19 infection at the emergency eye centre in Auckland.
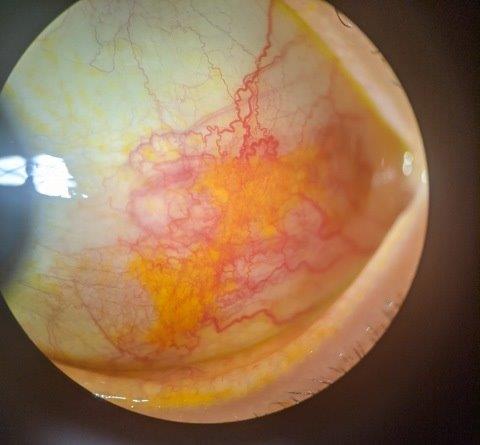
Fig 1. Scleritis following Covid infection
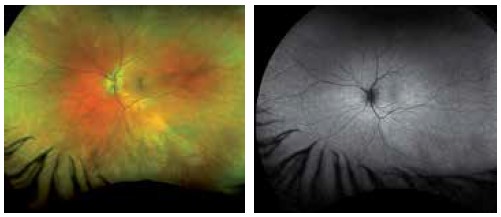
Fig 2a and 2b. Multiple evanescent white dot syndrome (MEWDS) following Covid infection
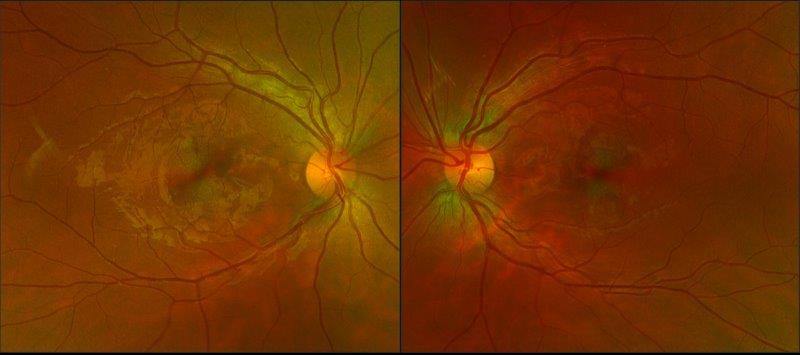
Fig 3. Acute macular neuroretinopathy following Covid infection (Optos image)

Fig 4. Acute macular neuroretinopathy following Covid infection (infrared image)
Endogenous endophthalmitis
Impaired immune status and intravenous access lines and catheters are risk factors for endogenous endophthalmitis. The literature reports 52 patients globally with acute respiratory disease secondary to Covid-19 and endogenous endophthalmitis, the majority of whom had multiple factors, with all receiving intravenous steroid treatment, type-2 diabetes in 60% of them, and most patients receiving intensive-unit care. It has been suggested steroid treatment may increase a patient’s susceptibility to opportunistic infections including candidosis (n=20) and aspergillosis (n= 2)7. The average time from infection to onset of visual symptoms varied from seven days to three months.
Retinal artery and vein occlusion
Covid-19 infection has been reported to predispose patients to multisystem thromboembolic events, including retinal vasculopathies including central and branch retinal vein and artery occlusion. There have been 15 cases of central or branch retinal artery occlusion reported in the international literature following Covid infection. The average age of presentation was 51 years, with one case associated with stroke and subsequent fatality. Interestingly, only a third of patients were hospitalised for Covid-19-related pneumonia prior, with the rest only having mild respiratory symptoms. At our institution an 18-year-old female presented with central retinal vein occlusion (CRVO) two weeks following positive Covid status with mild respiratory symptoms, with no other cause found on screening investigations (Fig 5).
There were 31 cases of central and branch retinal vein occlusion reported. Five cases of Purtscher-like retinopathy, a rare occlusive microangiopathy, were also described. The first case of CRVO was reported in a healthy 33-year-old man with mild respiratory symptoms and blurred vision8. Of all the cases described, only 10% were hospitalised for Covid-19 infection, with the majority first presenting to the hospital for eye-related symptoms including painless vision loss. While there was one case reported with concurrent deep vein thrombosis, this patient had underlying comorbidities which may be confounding. Nevertheless, this is in line with evidence of increased risk of venous and arterial thromboembolism in Covid-19 patients, with research required on the risk-benefit of anticoagulation9. Taken together, it is prudent to remember that patients with recent Covid-19 infection are at risk for ocular microvascular and systemic thromboembolic disease, which also includes stroke and pulmonary embolism. Furthermore, there may be value in performing Covid testing in young patients presenting with vein or arterial occlusions in the absence of identified risk factors.
Glaucoma
There has also been an association of acute angle closure with Covid-positive patients. At the Auckland Greenlane acute clinic, two patients presented with acute angle closure crisis. In both cases, the patients were hyperopic, of Chinese ethnicity and with Covid-positive status confirmed 24-48 hours prior to symptom onset. One patient had a simultaneous bilateral angle closure crisis. In one case report, all patients had hyponatraemia, which is thought to precipitate an angle-closure crisis in patients with shallow anterior chamber angles caused by osmotic pressure differences between blood and aqueous humour10.
Neurological sequelae
Covid-19-related optic neuropathy can present with painful or painless vision loss. There were 25 reported cases of optic neuritis internationally and 14 cases of other forms of optic neuropathy. For patients with optic neuritis (ON), the median age was 35 years, with bilateral involvement in 30% of cases. We also note that of the 25 patients reported with Covid-19-related ON, nine were found to have myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD)-positive ON. A significant proportion of MOGAD ON develop following a viral prodrome, so the association is not surprising. It is important to be aware of this association and ensure IgG-MOG antibody testing is performed. There were also two cases of first presentation neuromyelitis optica (NMO) following recent Covid infection11. In the 25 patients reported with ON, the majority responded very well to intravenous corticosteroids, with improvement in vision reported in all but four cases12.
Covid-19 infection occurs via angiotensin-converting enzyme 2 receptors, which are widely expressed in central nervous system cells, including the retina. It is postulated that there is an element of molecular mimicry in which Covid-19 antigens induce a significant host immune response, triggered by a cytokine storm (IL-1, IL-6, TNF-α), which activates glial cells and causes optic nerve demyelination13. Another hypothesis is that direct viral entry into the retinal nerve fibre layer may lead to endothelial cell dysfunction, causing coagulopathy or hypoxia13. The latter is a plausible mechanism for the development of non-arteritic anterior ischaemic optic neuropathy (NAAION), first described by Rho et al (2020)15, followed by nine other cases. At Greenlane, we have seen one classic case of NAAION in a 70-year-old female, with visual field loss on day 12 of Covid infection, although she had co-existing vascular risk factors (Fig 6). In one case report, a Covid patient developed NAAION in both eyes after receiving mechanical ventilation in the prone position, a well-established risk factor for NAAION16.
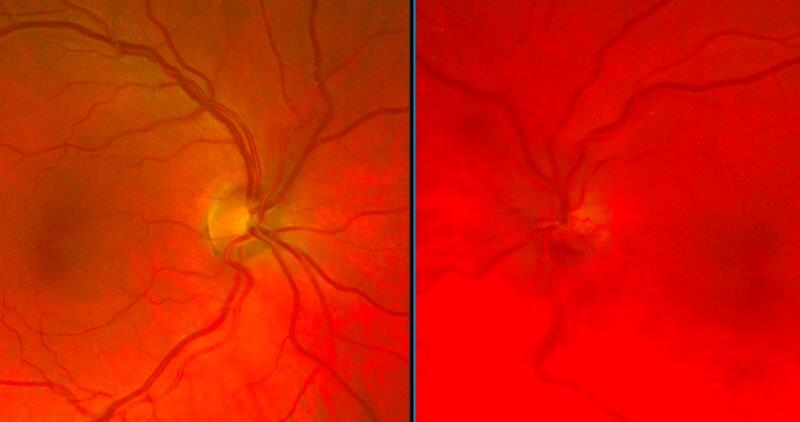
Fig 6a. Non-arteritic ischaemic optic neuropathy 12 days after Covid infection. Swollen left optic nerve with engorged retinal vessels
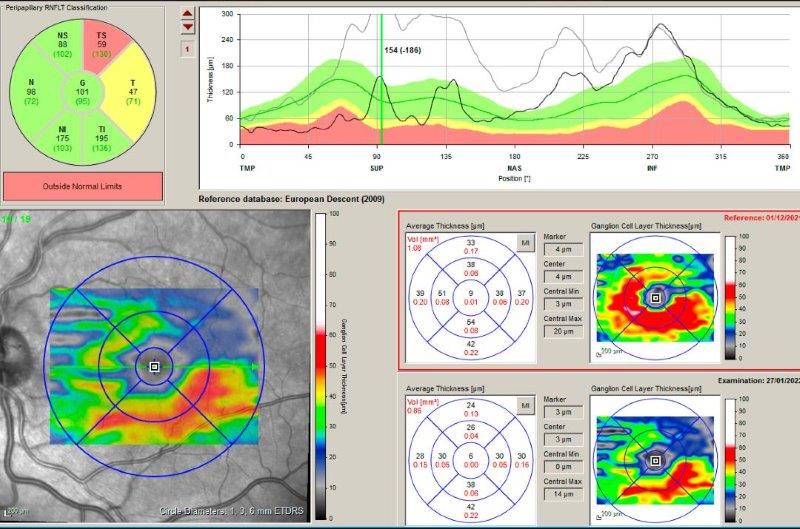
Fig 6b. OCT scan one month later showing resolution of nerve swelling, which was predominantly superiorly with superior ganglion
cell layer dropout
Any cranial nerve palsy can also be associated with Covid, with cranial nerves III, VI and VII being most commonly affected17. These can be single or multiple cranial neuropathies and can occur in patients with mild Covid symptoms, with and without other central nervous system involvement or other risk factors17. At Greenlane, a 57-year-old female with established vascular risk factors presented with a third cranial nerve palsy, with onset of diplopia on day zero of Covid symptoms.
Orbital sequelae
The most common orbital manifestation of Covid-19 was rhino-orbital mucormycosis, which presents with proptosis, severe pain, diplopia and vision loss. Similar to endogenous endophthalmitis, this condition is seen in critical or severe Covid-19 patients. All cases had other contributing features such as being immunosuppressed, having poorly controlled diabetes, being morbidly obese, or having low lymphocyte count. This is a life-threatening complication, requiring prompt identification and commencement of antifungals and/or surgical debridement for more extensive cases.
Conclusions
There is an increasing body of knowledge on how Covid-19 infection can lead to ocular diseases of varying severity. Increasing clinician awareness on the range of ocular symptoms during or after Covid-19 infection is essential to ensure patients undergo prompt ocular examination for early diagnosis and treatment of potentially sight-threatening disease. Care should be taken seeing patients with conjunctivitis in the community, due to the risk of undiagnosed Covid-19 infection. In addition, unusual clinical presentations as described in this report should prompt the astute clinician to consider Covid-19 testing.
References
1. Nasiri N, Sharifi H, Bazrafshan A, Noori A, Karamouzian M, Sharifi A. Ocular Manifestations of Covid-19: a Systematic Review and Meta-analysis. J Ophthalmic Vis Res 2021 Jan 20;16(1):103-112.
2. Chen Z, Yuan G, Duan F, Wu K. Ocular Involvement in Coronavirus Disease 2019: Up-to-Date Information on Its Manifestation, Testing, Transmission, and Prevention. Front Med (Lausanne) 2020 Nov 30;7:569126.
3. Wilkinson V, Sweetapple K, Niederer R, Chilibeck C. Manifestation of anterior necrotising scleritis and reactive infectious mucocutaneous eruption after Covid-19: a case report. N Z Med J 2022;136(1569):77-80.
4. Eser-Ozturk H, Izci Duran T, Aydog O, Sullu Y. Sarcoid-like uveitis with or without tubulointerstitial nephritis during Covid-19. Ocul Immunol Inflamm 2022 Feb 24:1-8.
5. Fischer N, Wann R, Crosson J. Acute posterior multifocal placoid pigment epitheliopathy following Covid-19 infection. American Journal of Ophthalmology Case Reports 2023;29:101790.
6. Adzic Zecevic A, Vukovic D, Djurovic M, Lutovac Z, Zecevic K. Multiple evanescent white dot syndrome associated with coronavirus infection: a Case Report. Iranian Journal of Medical Sciences 2023;48(1):98-101.
7. Agarwal M, Sachdeva M, Pal S, Shah H, Kumar R M, Banker A. Endogenous endophthalmitis, a complication of covid-19 pandemic: a case series. Ocul Immunol Inflamm 2021 May 19;29(4):726-729.
8. Yahalomi T, Pikkel J, Arnon R, Pessach Y. Central retinal vein occlusion in a young healthy Covid-19 patient: a case report. Am J Ophthalmol Case Rep 2020 Dec;20:100992.
9. Burn E, Duarte-Salles T, Fernandez-Bertolin S, Reyes C, Kostka K, Delmestri A, et al. Venous or arterial thrombosis and deaths among Covid-19 cases: a European network cohort study. The Lancet Infectious Diseases 2022;22(8):1142-1152.
10. Özmen S, Özkan Aksoy N, Çakır B, Alagöz G. Acute angle-closure glaucoma concurrent with Covid-19 infection; case report. Eur J Ophthalmol 2022 Jul 11:11206721221113201.
11. Caudill G, Wolin M. Myelin oligodendrocyte glycoprotein and neuromyelitis optica/aquaporin-4 antibody negative Covid-19-associated optic neuritis. J Neuroophthalmol 2021 Aug 2.
12. Mbekeani J, Raval N, Vo T, Rusu I, Lin S, Coyle C, et al. Purtscher-like retinopathy in a patient with Covid-19-associated coagulopathy. Arq Bras Oftalmol 2022;85(5):513-516.
13. Benito-Pascual B, Gegúndez J, Díaz-Valle D, Arriola-Villalobos P, Carreño E, Culebras E, et al. Panuveitis and optic neuritis as a possible initial presentation of the novel coronavirus disease 2019. Ocul Immunol Inflamm 2020 Aug 17;28(6):922-925.
14. François J, Collery A, Hayek G, Sot M, Zaidi M, Lhuillier L, et al. Coronavirus disease 2019-associated ocular neuropathy with panuveitis: a case report. JAMA Ophthalmol 2021 Feb 1;139(2):247-249.
15. Rho J, Dryden S, McGuffey C, Fowler B, Fleming J. A case of non-arteritic anterior ischemic optic neuropathy with Covid-19. Cureus 2020 Dec 7;12(12):e11950.
16. Clarke K, Riga V, Shirodkar A, Meyer J. Proning related bilateral anterior ischaemic optic neuropathy in a patient with Covid-19 related acute respiratory distress syndrome. BMC Ophthalmol 2021 Jul 13;21(1):276-9.
17. Finsterer J, Scorza F, Scorza C, Fiorini A. Covid-19 associated cranial nerve neuropathy: a systematic review. Bosnian Journal of Basic Medical Sciences 2022;22(1):39.
Dr Hannah Ng is an ophthalmology junior clinical research fellow at The University of Auckland (UoA), supervised by Dr Rachael Niederer. Her research focus is on streamlining intravitreal services in Aotearoa and her recent clinical experience includes a non-vocational ophthalmology registrar year in Auckland.

Dr Dan Scott is an ophthalmology junior clinical research fellow at UoA, supervised by Drs Rachael Niederer and Sophie Hill. His research focus is the clinical presentation, treatment and outcomes for diabetic retinopathy patients. Dr Scott has previous experience as a non-vocational ophthalmology registrar in both Gisborne and Hamilton and as a neuro-ophthalmology junior clinical research fellow in Auckland.

Dr Rachael Niederer is an ophthalmologist specialising in uveitis and medical retina, working at Greenlane Clinical Centre and Auckland Eye and is a senior lecturer at UoA. She has a special interest in Covid-associated eye disease and the ocular side effects of Covid vaccination.