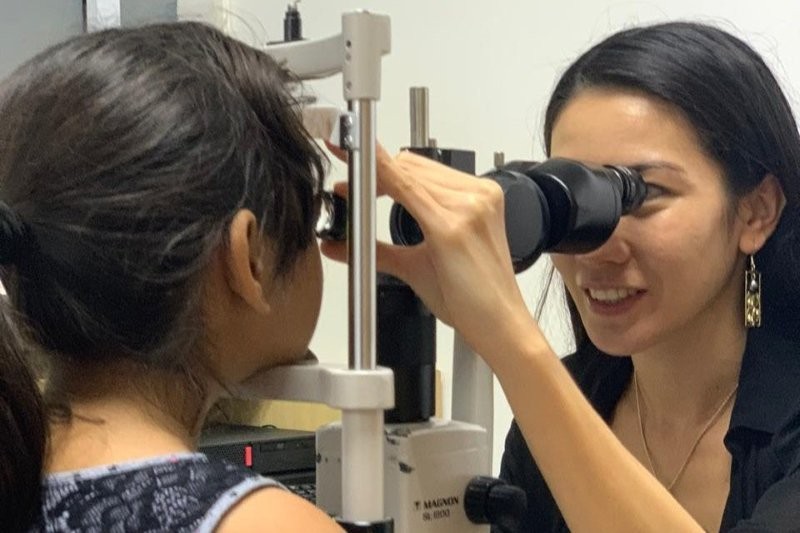
Meet the…nurse practitioner
There are 175 nurse practitioners (NPs) in New Zealand, but Carol Slight is the only one working in ophthalmology. Jai Breitnauer finds out more.
I meet Carol Slight on one of her non-clinical days at Greenlane Clinical Centre where she is based and, over a hot chocolate at Muffin Break on campus, discover just how busy Carol’s life is. She runs glaucoma clinics, uveitis clinics, works alongside several ophthalmologists and also goes off-site to assist at satellite clinics in other parts of Auckland, including Waitakere Hospital. She has her own patients, works largely autonomously, and is required to participate in 40 hours of continued, professional development education each year, which is audited by the Nursing Council every three years.
“It’s quite hard to become a nurse practitioner,” Carol admits, “It was a seven-year process for me. Perhaps that’s why there are so few of us.”
The role of nurse practitioner is relatively new. It was introduced in 2001 to help ease patient waiting times and manage an ever-increasing workload in our health care system. Nurse practitioners are registered nurses who have completed a masters in nursing, worked in an area at an advanced level for at least four years and are registered with the Nursing Council after an intensive portfolio assessment and oral interview. Nurse practitioners are registered in a specialist area, but still have a holistic approach to the care of patients. They bridge a care-gap for groups of patients who need expert assessment, but who do not require a consultant.
“I’m a hospital-trained nurse who qualified in 1980 and, apart from a few years out when I had my three children, I’ve always worked within an ophthalmology setting,” Carol says. “I wanted to further my skills, so I took a Masters of Nursing, and part of my dissertation was looking at the role an NP can play in relieving the pressure on waiting times for glaucoma referrals within a defined scope.”
Carol qualified as an NP in 2007 and began practicing in 2008.
The role of an NP is quite a lot more advanced than a registered nurse, even for those working in specialist areas, and Carol has made the job her own. But she stresses the collaborative nature of the work she does and the unique role she has.
“As an NP I can assess, diagnose and prescribe within my scope of practice. I see, and treat, a lot of patients – in fact I probably see more uveitis patients through my clinic than many junior doctors. But I also work very closely with ophthalmologists and I learn a lot from them.”
Carol also says as a nurse practitioner you have to be both confident in your skills and know where the boundaries of your role end. This is important, not just for the safety of patients, but also to maintain a good working relationship with other healthcare professionals – some of whom may not fully understand the scope and skills a NP has.
“I get referred the lower-risk patients, or patients who are transferring from private to the public system. I do initiate treatment under some circumstances, and it is possible for me to see a whole patient episode-of-care without having to involve anyone else, however, there are certain sub-specialities I feel more comfortable in, and certain things I don’t do by choice. For example, I don’t give Avastin injections for AMD patients although that could always be a possibility if I underwent the training and audit process.”
Anything related to narrow-angle glaucoma, laser treatment or patients with a complicated condition, or who perhaps need surgery, are also referred quickly to a consultant if they end up in one of her clinics, she adds.
“I have consultants I can call on, and I have a lot of support. It’s about buy-in, and getting that comes through cultivating trust. They know I won’t push my boundaries.”
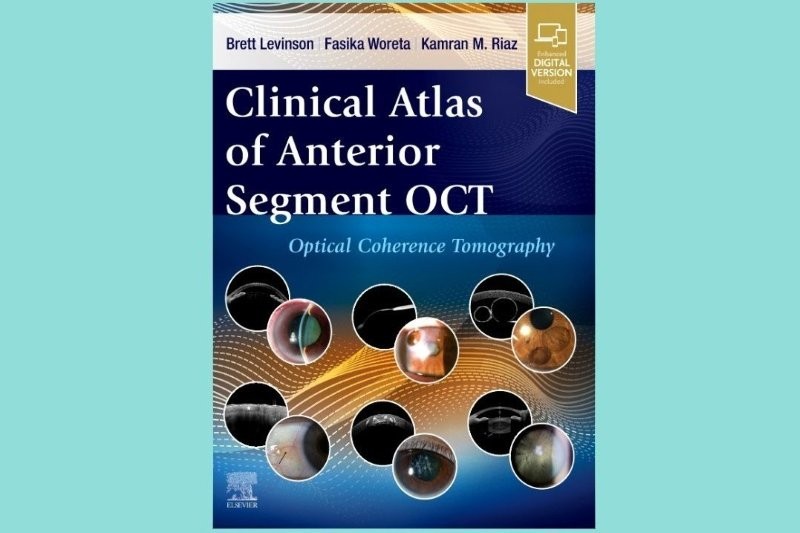
One of the biggest challenges for Carol is her requirement for continuing education. As the only ophthalmology NP in New Zealand, she finds her needs aren’t necessarily catered for by current educational programmes.
“At the RANZCO conference, I spent more time in the doctors’ conference than in the nurses’ room,” admits Carol, who was a speaker at the nurses’ meeting this year. “I do get some additional funding to attend overseas meetings and events, as I don’t always get what I need from local programmes. I’ve previously been to the World Glaucoma Congress in Hong Kong and Canada, and I’m hoping to go to the International Ocular Inflammation Society conference in Switzerland next year.”
Another issue Carol has to face is making sure other professionals understand the full scope of her role, although this is a journey all NP’s have to face, she says, particularly when undertaking roles that traditionally have been the domain of medics.
“As trailblazers we’ve all had to pave the way, but I think we’ve all found it has run smoothest when we work alongside someone more senior as a mentor.”
Carol says she’s grateful for the support she has had within ophthalmology circles in Auckland. “The scope of my role is increasing now, and also the understanding of what I do is getting wider. I have recently worked with ophthalmologists in other parts of New Zealand on working groups looking at elective surgery prioritisation.”
Ultimately, the part of the job Carol most enjoys is its personal nature; seeing patients regularly, helping them and making connections.
“I had patients who were with me through the birth of my first grandchild. These patients always ask how many grandchildren I have now. My patients share things with me as well. You make friends, build personal relationships, and live through the highs and lows of their lives.”