OA22: from wellbeing to orthoptic-led clinics
The sun was shining and you could feel the excitement as the 78th Orthoptics Australia annual conference kicked off at the Brisbane Convention & Exhibition Centre. More than 200 orthoptists from around the country gathered for the first face-to-face conference in three years, which delivered a highly engaging scientific programme over the three days with outstanding presentations, new research and technology.
Before diving into the clinical side, we were eased into the first morning with a brilliant reminder about the importance of self-care from Alison Coughlan, an expert in health and social workforce wellbeing. In what has been a tough few years working through a pandemic, she explained how we can recognise the signs of burnout and prevent it.
Let’s get clinical
The highlights for me were the talks relating to paediatric ophthalmology, with the Sydney Children’s Hospital’s orthoptists well represented as they delivered their fascinating case studies. Among them was Coco Howard, whose talk was on demyelinating disease in childhood/juvenile-onset multiple sclerosis (MS), which represents 2-10% of MS cases. Another case study involved a 15-year-old girl who presented with blurred left vision and painful eye movements and, with a significant family history of MS, was a suspect for optic neuritis. Further investigation with MRI demonstrated multiple T2-weighted-fluid-attenuated inversion recovery (T2/FLAIR) lesions, with one mildly enhancing lesion (dissemination in time).
Howard went on to describe how OCT can be used to help monitor axonal degeneration for optic neuritis patients, since the condition results in a loss of retinal ganglion cell axons, which is easily monitored using the OCT machine’s retinal nerve fibre layer (RNFL) and optic disc report.
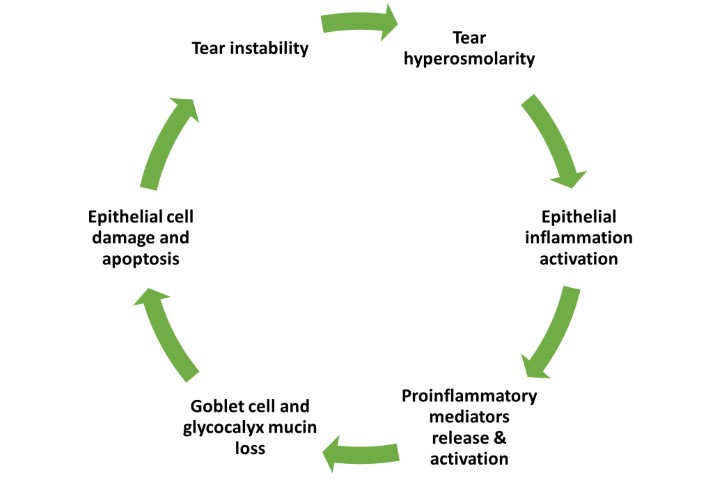
Orthoptist at The Children's Hospital at Westmead Stephanie Crofts presented on juvenile idiopathic arthritis (JIA), uveitis and a multidisciplinary care approach. JIA affects 1 in 1,000 kids under the age of 16 in Australia, impacting one or more joints for at least six weeks. JIA uveitis accounted for approximately half of all paediatric uveitis and 30% of JIA patients will develop the condition – commonly chronic anterior uveitis that is bilateral and asymptomatic. As uveitis symptoms in kids with JIA are silent, it is important to monitor high-risk JIA patients every 3-4 months.
Crofts’ colleague Georgia Shaw presented on the alarming number of traumatic eye injuries in paediatrics, affecting six million children per year. Of these, 250,000 need to be hospitalised, 3.9 million suffer bilateral vision loss and 1.8 million suffer monocular vision loss. This costs the Australian Government AU$155 million per year. The obvious reasons traumatic eye injuries are higher in the paediatric population than in adults is their inability to perceive risk, lack of physical coordination and vulnerable facial morphology. The impacts of trauma are also more severe than in adults and can lead to amblyopia as well as reduced quality of life. Children whose injuries extend to the lens also have poorer visual outcomes. Shaw’s case studies involving eye-penetrating objects, such as a pencil, a satay stick and a Stanley knife, were accompanied by gory images, which had us squirming in our seats!
Ginkgo biloba, Braille and baristas
The OA conference programme was cleverly designed so we could join our ophthalmologist friends for lunch in the RANZCO exhibition hall, where we could test some of the latest tech and ophthalmic devices. It didn’t hurt to have a barista-made coffee and some Messina gelato available, too!
The rest of the afternoon consisted of talks on the retina and low vision, a highlight being the use of Lego bricks to assist low-vision children to learn Braille through play, which I think is a brilliant collaboration with the toymaker.
The morning of day two focused on general ophthalmology and glaucoma. I found Melbourne-based Royal Victorian Eye & Ear Hospital’s Dr Brian Ang’s talk on the neuroprotective benefits of Ginkgo biloba leaves for normal-tension glaucoma (NTG), super interesting. The plant has been used since ancient times and may be a complementary treatment to reduce the rate of glaucoma progression for patients with low intraocular pressure (IOP). Studies of Ginkgo biloba extract’s effect on NTG found that it slowed visual field progression over the long term. Other studies found that, compared to placebo, Ginkgo biloba helped improve pre-existing visual field damage in NTG. It also provides antioxidant and anti-inflammatory effects, mitochondrial stabilisation, an increase in microcirculation to improve endothelium-dependent vasodilation and reduces blood viscosity. The risk of bleeding with Ginkgo biloba extract, however, is often overstated based on case reports, he said, and has not been demonstrated in most trials and meta-analysis.
Dr Ang’s presentation demonstrated the benefits of a proactive approach to managing glaucoma suspects and patients through nutrition and lifestyle changes – contrary to the current approach of monitoring them every 6-12 months and only taking action once progression has been confirmed. I’m all for supplementing through nutrition as an alternative to drugs where we can, so I know which path I would prefer.
The afternoon covered genetics and models of service delivery, with orthoptist-led clinics being a main point of focus to help reduce the burden on health systems and wait times for patients, while producing a cost-effective and patient-focused solution. It was great to hear former OA president Marion Rivers’ talk on the introduction of a national set of minimum standards for preschool vision screening in Australia. This was implemented well in New South Wales’ StEPS programme and is being used as a case study to adopt a similar model across Australia. It will ensure all 3.5-5-year-old Australians have access to integrated and people-centred eyecare, where vision-screening programmes with coordinated pathways for referral and follow-up will help with early detection of vision problems and facilitate timely treatment.
I’m a huge fan of this framework and I commend the hard work of all involved to create this change; it’s just a shame this wasn't implemented nationwide by the government sooner, when StEPS started. My only concern is a potential lack of consistency among the different states in the way they collect and use data, which will hinder the reporting of prevalence and prediction of trends in children’s eye health. If they can create a standardised system nationwide for this, we’ll be onto a winner.
The conference wasn’t all clinical, however, with the highly anticipated OA masquerade dinner seeing everyone frocked up and rocking some clever and creative masks. It was also an opportunity to welcome new OA president Dr Amanda French and celebrate excellence in the profession, with Caleb Bartolo taking the Emma Russell Prize, Sarah Harkins the Paediatric Award, Coco Howard the Delegate’s Choice Award and Jane Schuller winning the Zoran Georgievski Medal.
I had a wonderful time as an attending orthoptist and as an exhibitor, catching up with friends and colleagues. Congratulations to the Orthoptics Australia team on a wonderful conference that was so well organised and informative, and left us all eager to attend the next one.

Maddy Scavone is an orthoptist specialising in paediatrics and founder of Speckles, a company focused on children’s vision needs and wants.