Optometry Australia calls for collaborative care pilot
Against a backdrop of potential Medicare funding cuts for anti-vascular endothelial growth factor (anti-VEGF) injections, Optometry Australia (OA) has urged the nation’s major political parties to commit to investing AU$1 million over two years in a collaborative-care pilot study to more effectively deploy Australia’s optometry workforce and improve eyecare access.
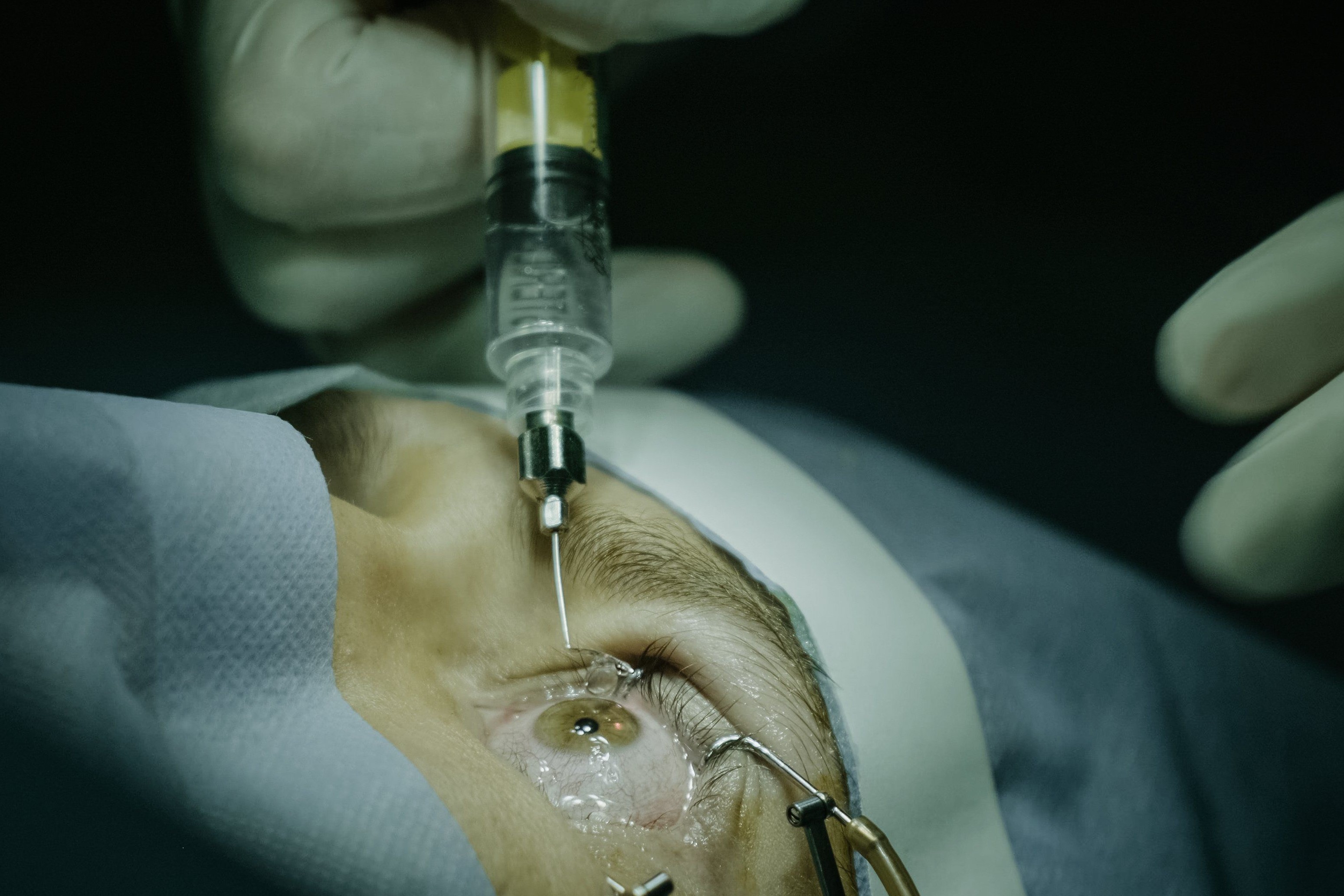
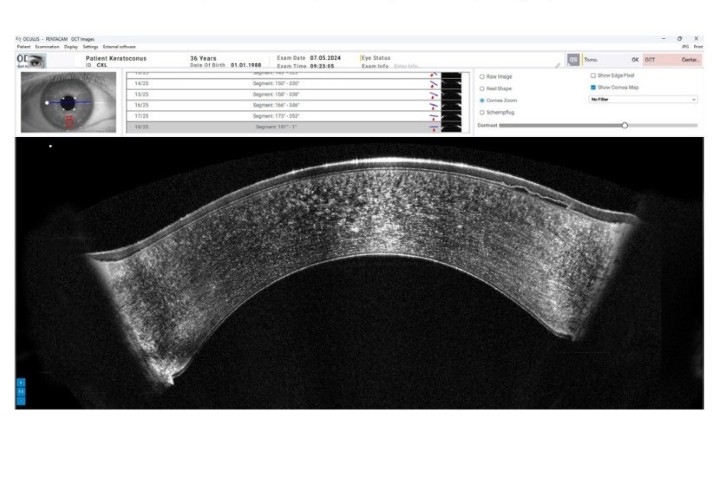
OA proposes allowing skilled optometrists to collaborate with ophthalmologists to treat patients with age-related macular degeneration (AMD) and diabetic macular oedema (DMO) across two locations, including a remote Indigenous community. “Although these patients require regular treatment, often administered by intravitreal injection, access can be difficult if ophthalmic care is not readily available due to location or cost. It is therefore understandable that there is a 20% drop-out rate for intravitreal injection treatment,” said Murray Smith, OA president.
In Australia there are significant barriers to intravitreal injections, resulting in people missing out on treatments that save their vision, OA optometry development manager Ben Hamlyn told NZ Optics.
“I suspect that similar issues are faced by patients across New Zealand. In Australia, intravitreal injections are delivered almost entirely by ophthalmologists and in areas where there are fewer ophthalmologists there are fewer intravitreal injections taking place. Two of the most profound barriers to intravitreal injections in Australia are access to ophthalmologists and out-of-pocket expenses for the patient when they do have treatment with the ophthalmologist,” said Hamlyn. “The current funding structure in Australia incentivises an inefficient use of ophthalmologists’ time, undertaking tasks that could be safely undertaken by other health professionals.”

Ben Hamlyn, OA optometry development manager
The call for the pilot study is backed by the Australian College of Optometry (ACO), which has already seen the success of such partnerships, said Pete Haydon, ACO CEO. “For the past six years, we’ve worked with the Royal Victorian Eye and Ear Hospital’s glaucoma collaborative care clinic to alleviate pressure on in-demand ophthalmologists and, most importantly, ensure access and equity for patients in a timely manner.”
While OA members are keen to extend their scope of practice, it would not be for everyone, said Hamlyn. “More and more optometrists are working within public hospitals and alongside ophthalmologists in private ophthalmology in retinal clinics. We expect optometrists who work in these settings would be the ones who undertake the training to enable them to take on this treatment within these settings, as well as optometrists in regional and rural areas where, currently, access is particularly fraught.”
To increase access to anti-VEGF injection treatments for patients across Australia, in the face of maldistribution and expected undersupply of ophthalmologists, the Medicare Benefits Schedule (MBS) Review Taskforce recommended the Medicare rebate for eye injections should be cut by 70% and, mirroring what happens in the UK, that “appropriately trained” nurse practitioners and optometrists should be allowed to extend their scope to give injections*. The recommendations were welcomed by OA but caused an outcry from the Australian Society of Ophthalmologists and RANZCO. Despite strong safety evidence from both the UK and New Zealand in support of this change, and its cost savings and patient benefits within the public health system, an ophthalmology-led lobbying campaign ensued. Backed publicly by the Macular Disease Foundation of Australia (MDFA), the campaign led to both Australia’s main political parties rejecting the proposed recommendation at the start of May.
While treatment access and costs are obstacles for AMD patients, a recent Australian survey also highlighted a lack of awareness of anti-VEGF treatment, despite it being available for 15 years. The YouGov poll of Australians aged 50-70, commissioned by MDFA, found that fewer than one in 10 were aware of intravitreal injections. The survey also found vision is the sense Australians value most, with the fear of going blind (45%) rating higher than losing memory (40%), a limb or mobility (17%), hearing (6%) and speech (2%).