Teaching optometry’s future
The new head of the School of Optometry and Vision Science (SOVS) at Auckland University, Dr Andrew Collins officially assumed the role on Good Friday this year. Was that a good omen? Lesley Springall sat down with him to find out.
Was Good Friday 2022 a good Friday for you?
DR COLLINS: It’s an interesting question. Steven (Professor Steven Dakin, former head of SOVS) always used to joke that his first day was 1 April. So I think Good Friday has to be better than that!
Are you excited about the move from academic director to head of school?
I genuinely think so. I had to think about it before I applied, but I thought I had something to offer and it was an opportunity to grow in my own role. I am passionate about where optometry is going and we have a great mix of clinicians and vision scientists, which gives us the opportunity to address a wide range of issues and research areas.
How important is the vision research side of optometry teaching?
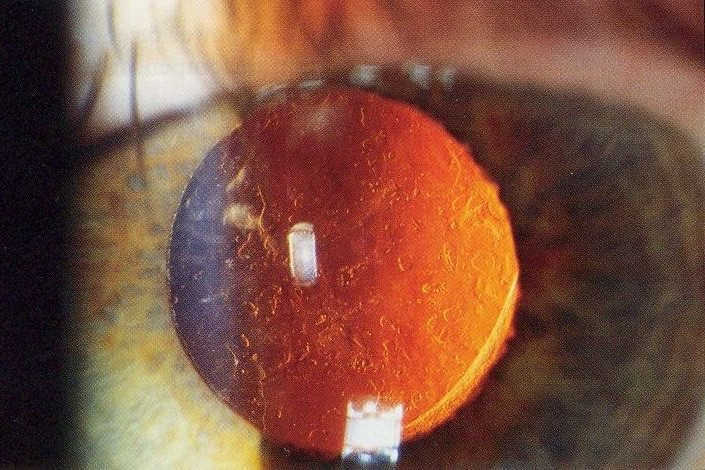
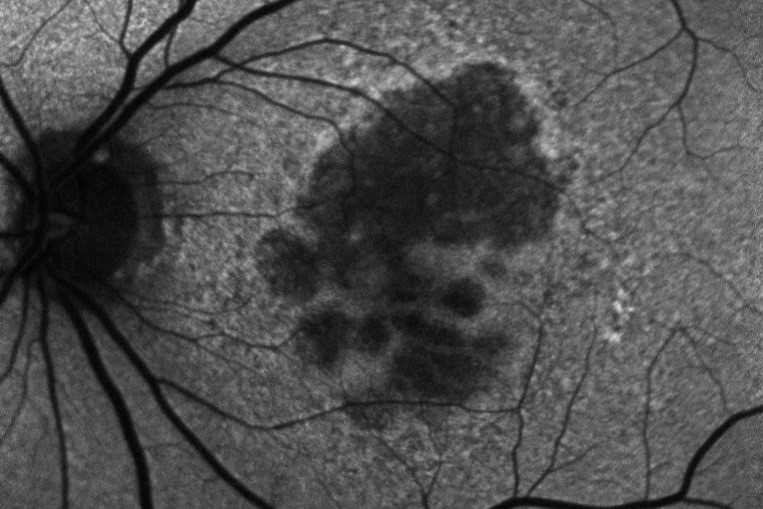
It underpins our clinical teaching, our understanding of why we do certain things. Think about conditions like age-related macular degeneration (AMD). We teach students what it looks like, who’s likely to get it and how to detect it, then what the potential treatments are and why, when and where they should refer. But we also make sure we teach the students what AMD is – what is actually happening in the retina – so they can better understand the risk factors and what the underlying disease process is. Some go on to consider postgraduate research, so they can translate basic research through to clinical care and back again. It’s really good cross-pollination; the two support each other, which is really important.
Are you still a registered optometrist?
Yes, I keep up my CPD. I think it’s important, to provide leadership, to understand what the current role and scope of an optometrist is, but it’s not essential. Other heads (who aren’t registered optometrists) bring different perspectives. Steven, being a vision scientist, obviously strongly supported vision science, but he also grew community optometry with the appointment of Jacqui Ramke (community eye health researcher at Auckland University and Associate Professor of Global Eye Health from the London School of Hygiene and Tropical Medicine), who went from clinical practice as an optometrist to population health research.
These associations are important. Leon Garner (foundation professor of optometry at Auckland University) was an engineer before he became an optometrist and he developed a very close association between optometry and engineering, which continues to this day with people such as Jason and Ehsan*. Because, if you think about how the eye works, you have to understand light, optics, biochemical mechanisms, molecular biology and perception, which is where other aspects, such as neuroscience and psychology, come in. Optometry spans a wide range of sciences, which is why it’s important to have strong cross-pollination between the various groups.
*Dr Jason Turuwhenua, a senior research fellow with the Auckland Bioengineering Institute who’s currently co-developing novel technology to identify visual acuity issues in young children; and Dr Ehsan Vaghefi, who completed a PhD in biomedical engineering at Auckland before founding AI tech firm Toku Eyes.
What’s the biggest change you’ve seen since you qualified?
When I graduated, we had just started doing diagnostic optometry. Then I retrained, together with many others in the mid-2000s, to provide therapeutics, which was a big advance. Later, we became authorised prescribers, which put us on the same level of prescribing as a GP but within our scope. And now, the latest scope change is enabling hospital optometrists to provide limited laser surgery¹. It’s a very exciting time and an incredible expansion from where I was 25-plus years ago.
One of the most exciting things is seeing the expansion of optometrists’ role to becoming health practitioners in the real, true meaning of the words.
We’re ahead of Australia in this regard, but still behind the UK, where hospital optoms have been providing services such as anti-VEGF injections for many years
I have a hospital optometrist friend in the UK who runs his own clinics. He’s not just delivering treatment, he’s deciding who gets treatment as well, so that’s very exciting. We supported the YAG laser scope change¹ and we’d support further scope changes. It’s important to recognise the range of skills optometrists can have and the benefits they can bring to the health system.
But not all optometrists will want to take this path?
No. Some are clinically minded and some are more business minded; we’ve got a very broad range, but they all get the same training, then it’s up to them where they take it. But it’s important to recognise the changes occurring in the health system which will open up opportunities for optometry. There are already examples of optometrists in private practice seeing publicly funded glaucoma patients. That’s the type of seed that can grow. It would be great if optometrists could one day be considered the primary healthcare practitioner of the eye.
Is SOVS supporting the New Zealand Association of Optometrists and others who are lobbying the government for change?
Yes, through Eye Health Aotearoa and other avenues. Optometry is a community resource and everyone is now talking about how you get services out to the community, which optometrists are well placed to do. If there was public funding, it would also significantly improve access to eyecare for everyone.
Isn’t SOVS’ new Vision Bus designed to address some of these issues?
Yes, it provides a clear example of what can be done. We are not only training our students to be clinicians, we also want them to understand the environment in which they're operating, to understand the communities they're going to be working in and some of the barriers to access they face in the way optometry currently operates. It's also about research; data around the vision status of New Zealanders are lacking. If we’re talking about refractive error, we often have to quote numbers from Australia because we simply don’t have them here; we don't even know what proportion of New Zealanders have myopia, so the Vision Bus is part of that too.
There are concerns from optometry around dispensing opticians (DOs) becoming contact lens prescribers as they are in the UK. Where does SOVS sit on this?
I wouldn’t want to restrict anyone from their dreams. What I’m interested in is a healthcare system that provides the best possible access and service to the public by whoever is part of it. Dispensing opticians may well have an expanding role in this.
Would you consider expanding SOVS’ programmes to train DOs?
There is a shortage of trained DOs in New Zealand and, unlike Australia, they are regulated health providers here, but there are only so many things we can do as a school with the funding provided. With the recent (optometry) scope changes, we’re putting our efforts into creating a highly skilled, broadly educated optometric workforce that can operate in the future health system, because I think we really are on the cusp of change.
Under the university’s new strategic plan, all departments are reviewing their curriculums to make them more future focused, more transdisciplinary; we’re removing the silos in the organisation. This is very important for optometry because it crosses so many disciplines. Take education: children need good visual function to perform well at school, so how can educational theory and practice inform what we do in optometry and vice versa? It’s these crossovers that you will see reflected in the new curriculum.
Is it hard to pull all this together when we don’t even know what shape Health NZ will take?
I’m very much in support of Steven's work into the public health aspect of optometry, because it addresses where optometry can be in the future. If we understand what the needs are, then optometrists can be part of the solution. The pandemic threw up lots of interesting examples of this, like the immunisation drives – we literally saw people going door-to-door. It showed how one size doesn’t fit all; you really need to understand your community to provide the best possible care.
Do you think optometrists should call themselves ‘doctors of optometry’ (OD)?
I know some dentists call themselves doctors and some vets do too, but it’s basically an honorific. What’s most important is there is no confusion about it. Most (optometry) school students in Australia graduate now with master’s degrees because they have this dual structure, combining bachelor’s and master’s, so the question is, why aren’t we doing that?
We currently have a bachelor’s degree that takes five years and is awarded with honours. That’s a very long bachelors’ degree, so it’s a bit of an odd one. We could change this to the three-plus-two Australian model, which would retain the same sort of entry requirements we currently have and splits nicely into preclinical and clinical, which we already have. The alternative is what we see in Melbourne and the new doctorate course in Western Australia², which is graduate entry and a four-year named doctorate, an OD degree, similar to what you see in the US. But I think it’s most likely (it will be the former) as that fits most easily with what we currently do.
Optometry started as a two-year diploma, then it changed to three years, then a four-year Bachelor of Optometry and now it’s five years as we’ve had to increase the content and training. It’s important for students to be recognised for what they do.
If you had a magic wand what would be the one thing you’d change in eyecare in NZ today?
I would improve access, probably by providing public funding for optometry.
And what is the one thing you hope every SOVS optometry student takes with them when they graduate?
Understanding their wider role as a healthcare professional in the community. You can be a very good businessperson, you can be very good at refraction and you can be very good at focusing on ocular health and prescribing, but what’s most important is understanding that it’s a role involving people and providing the best possible health service you can for them.
- https://www.nzoptics.co.nz/articles/archive/yag-laser-optometry-scope-change-approved/
- https://www.nzoptics.co.nz/articles/archive/new-doctor-of-optometry-degree-accredited/