ANZSS flexes its muscles
It gave me great pleasure to attend this year’s Australia and New Zealand Strabismus Society (ANZSS) meeting in Sydney. Held at the beautiful Art Gallery of New South Wales, the programme was rich in academic content, delivered by outstanding speakers. As a strabismologist, every presentation was acutely relevant to my own practice.
Professor Linda Dagi from the Boston Children’s Hospital (BCH) kicked things off. For such a petite woman she was a real force of nature, delivering five captivating lectures over the two days. She spoke about treating partial and complete third-nerve palsies, delighting us with novel techniques for splitting the lateral rectus and transposing each half nasally to the medial rectus. In her William Gilles Lecture, she told us about “the tilt you see and the tilt you don’t” in cases of torsional strabismus, be they of neurologic, mechanical, orbital or iatrogenic origin, such as from previous surgery. She warned us not all Parks-Bielschowsky-positive manoeuvres were due to fourth-nerve palsies and a tight inferior rectus could also yield a positive test.
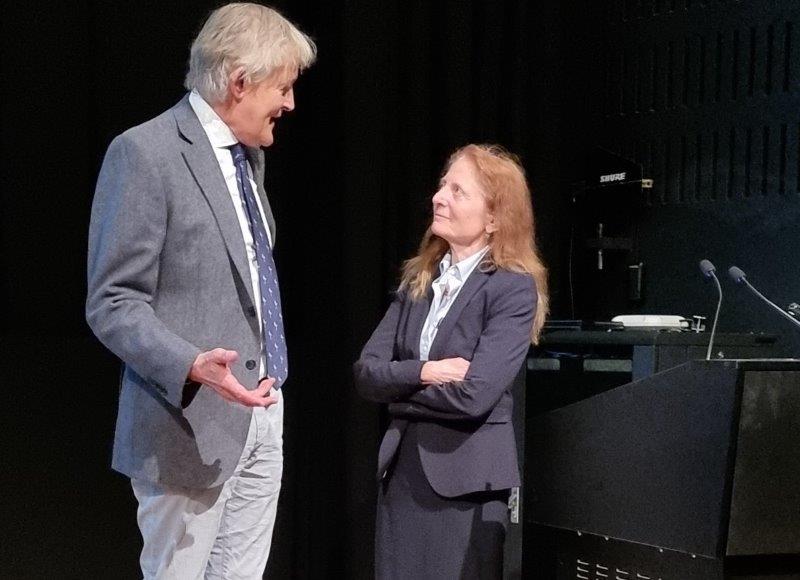
Profs Mark Gillies and Linda Dagi
A world expert in craniosynostosis-related strabismus, Prof Dagi revealed that when patients with craniosynostosis have open cranial vault expansions and orbital advancements, the trochlea is moved way back, giving rise to even more complex ocular deviations than those originally present. Recently, a minimally invasive endoscopic approach at three months of age has been developed to reshape the skull instead. It’s a much quicker procedure, has a better risk profile and may not exacerbate the strabismus as much as the traditional open approach, she said. However, this new approach is not yet widely available.
‘Adjustable’ surgery
Prof Dagi also discussed surgical treatment of Duane syndrome and sixth-nerve palsies. She combines a medial rectus recession with a superior rectus lateral transposition, using adjustable augmentation sutures to reduce excyclotorsion induced by transposition. Her procedure included placing sutures with a scleral bite at 6mm, 8mm and 10mm from the lateral rectus insertion, which can then be selectively removed postoperatively if the desired effect on torsion is too great. She cautioned against recessing the medial rectus too far as this limits convergence, which patients find very disabling.
With regard to vertical strabismus in thyroid orbitopathy, Prof Dagi clarified when to recess one inferior rectus and when to recess both. She also gave us tips on how to avoid late overcorrection. She stressed the importance of leaving the patient with good binocular single vision in primary position and in downgaze. Ideally, their post-operative head position should be of a slight chin-up attitude so that they can descend stairs safely. Finally, she spoke about the new “miracle drug” teprotumumab (Tepezza) for thyroid orbitopathy. It reduces the size of the extraocular muscles and proptosis, and reduces strabismus in 67% of patients. Unfortunately, upon stopping treatment, the disease flares up again in 40% of patients. Many patients also withdraw from treatment due to adverse effects such as hearing loss, muscle spasms, nausea and diarrhoea. It is also highly teratogenic. Teprotumumab was US Food and Drug Administration approved in 2020 but is not yet available in New Zealand.
ANZSS’ other guest speaker was Professor Gillian Roper-Hall from the St Louis University School of Medicine in Missouri. Prof Roper-Hall eloquently educated us on the history of extraocular muscle transposition surgery, which dates back to the 1880s. She then discussed diplopia management in adults with neurodegenerative or musculoskeletal disorders. Due to their inability to maintain a neutral and upright head position, a surgical aim of achieving single vision in the normal primary position may not be appropriate or useful to these patients. Therefore, the aim of strabismus surgery here is to get the eyes straight in the patient’s best gaze position. Other measures, such as the ‘lazy readers’ available online, can be of great help to someone who can’t look down or who has nystagmus in downgaze. Using prisms, these glasses shift an image upward, obviating the need to tip the head downward. Choosing the best glasses for a patient is also vital, with single vision being best, she said. But if progressive lenses are required, it is preferable to use them for intermediate and near vision rather than for distance.
Eyes front!
Prof Roper-Hall also spoke about the ‘unique oblique’, demonstrating the phylogenetic origins of the superior oblique muscle. Starting with fish with eyes on either side of the head, she related these origins to the muscle’s current functions in forward-facing eyes. The superior oblique muscle is implicated in numerous abnormal eye movements, including congenital and acquired Brown’s syndrome, superior oblique click, myasthenia gravis, superior oblique myokymia and the rare disorder, ocular neuromyotonia. Finally, Prof Roper-Hall discussedirregular forms of diplopia, including paradoxical diplopia, visual confusion, binocular blurring, diplopia with visual-field defects, foveal displacement syndrome, intractable diplopia and the very rare monocular diplopia.
But Squint Club (as it’s more affectionately known) would not be Squint Club without the live cases. The first was a seven-year-old boy with infantile nystagmus, alternate esotropia, foveal hypoplasia and slight face turn to the left. It was interesting to see the panellists differ in their advice for best surgical procedure. One preferred bilateral medial rectus recession while two others recommended a resect/recess procedure.
The next case was longstanding superior oblique palsy with minimal phoria in primary position. This time the panellists agreed on recommending inferior oblique weakening. A more challenging case of Apert syndrome with V-pattern exotropia and vertical squint was next. This child had previously undergone cranial, orbital and squint surgeries. Prof Dagi suggested transposing the already recessed inferior oblique muscles nasally as that would convert them from extorters to intorters. Clever tip, I thought! Another case involved a 38-year-old lady with dual pathology of right fourth-nerve palsy, left third-nerve palsy, anti-thyroid peroxidase antibodies and an exquisite responsiveness to selenium. Although an explanation proved elusive, I resolved to replenish my stock of Brazil nuts.
As for our own Kiwi presenters, Greenlane paediatric ophthalmology fellow Dr Tiffany Ma elegantly presented a baffling case of recurrent painful ophthalmoplegic cranial neuropathy without pain, as well as a case of postoperative and enduring astigmatism following squint surgery. Many of us were left wondering how often we’ve been guilty of inducing astigmatism too. Auckland University’s Dr Sarah Hull presented her case of complex vertical strabismus after stroke in a high myope. Though the patient was insistent on further squint surgery to improve cosmesis, the consensus was that she didn’t look too bad and further surgery was not indicated. Finally, Dr Robert Barrett, paediatric ophthalmology fellow at Counties Manukau SuperClinic, presented a case of postoperative double elevator palsy with what appeared to be progressive ipsilateral ptosis. He was advised to investigate the ptosis further and, if no sinister cause was found, proceed with ptosis surgery as, ultimately, the patient just wanted to look more ‘normal’.
Other memorable events from the meeting were a video on Professor Frank Martin’s awe-inspiring career; a tribute to Dr John Pater from Adelaide Women's and Children's Hospital, in recognition of his dedication and contribution to strabismus and paediatric ophthalmology; plus a fabulous dinner in which both keynote speakers were presented with Aussie Akubra hats as a heartfelt thank you for their contributions to ANZSS 2023 – a brilliant touch! Melbourne has a tough act to follow when it hosts ANZSS 2024.

Dr Julia Escardó-Paton specialises in paediatric ophthalmology and strabismus in Te Whatu Ora Auckland and Counties Manukau, and at Eye Doctors. She obtained her undergraduate degree in the US, her medical and ophthalmic qualifications in the UK and her paediatric ophthalmology and strabismus fellowship in Auckland.