Capacity constraints blamed for mans sight-loss
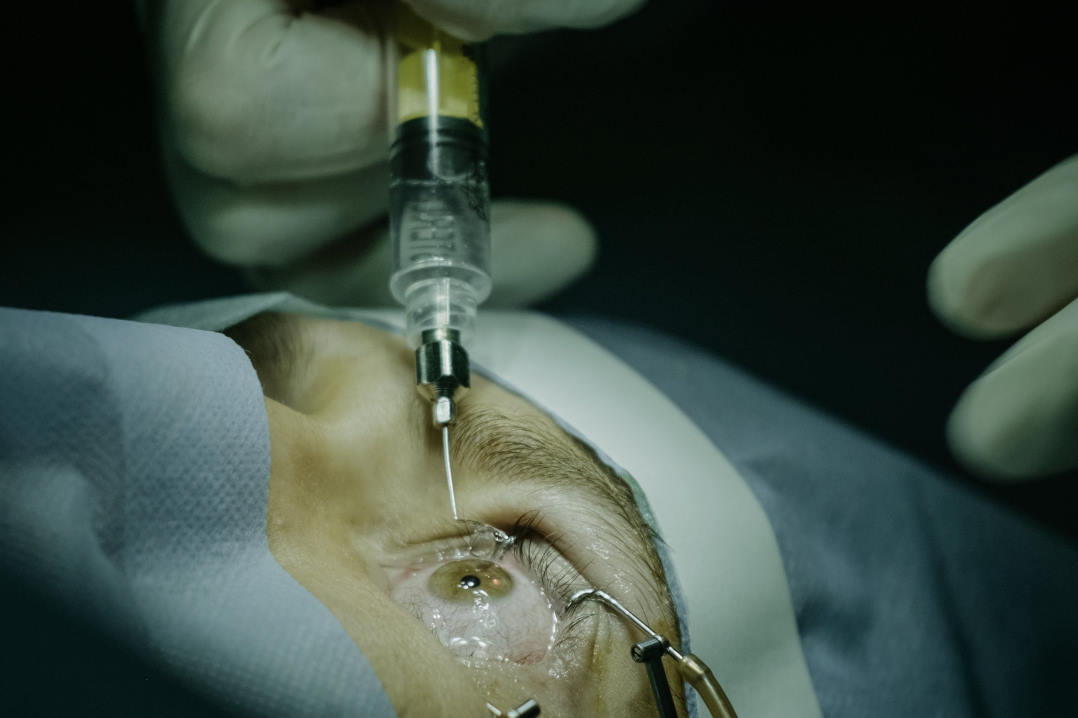
A Canterbury man with neovascular age-related macular degeneration (nAMD) permanently lost sight in his right eye after a delayed follow-up for anti-VEGF injections, according to a Health and Disability Commissioner (HDC) decision. The delay followed the patient, previously stabilised on aflibercept treatment under private care, being transferred to Health New Zealand Waitaha Canterbury.
At a March 2022 consultation, the patient’s regimen was extended from monthly to three-monthly. Clinic notes recorded “stop injections” and a three-month follow-up, but no appointment was made. Despite contacting the service in September 2022 after noticing visual change, the patient received a generic waitlist delay response. Having later been advised to seek reassessment, the patient’s private specialist confirmed irreversible macular damage in April 2023. Health New Zealand apologised, acknowledging that the delay allowed the macula to ‘blow out’. The HDC report was released in November 2025.
Independent advice to the ACC from the University of Auckland’s Professor Helen Danesh-Meyer found that required standards of care were not met and review timeframes were unacceptable and directly responsible for the failure of the patient to receive adequate treatment.
The decision noted longstanding warnings from the ophthalmology service, with clinicians repeatedly escalating concerns about capacity, overdue follow-ups and avoidable harm. The district’s waitlist remained severely constrained, with thousands of overdue patients and sustained specialist shortages, it said. The HDC found Health New Zealand Waitaha Canterbury in breach of Right 4(4) for failing to minimise harm.
Health New Zealand Waitaha Canterbury cited a high turnover of senior medical officers (SMOs) as causing difficulties managing the service as new SMOs are appointed. “First specialist assessment (FSA) waiting list is currently 1,115 – of which 50% are waiting longer than 120 days to be seen. Of those waiting for vitreoretinal surgery, 80% of FSAs for this group are overdue – the service can only see immediate and urgent currently. The positive aspect of the service is in relation to the surgical waiting list with >70% waiting less than 120 days. This is largely due to outsourcing, of which 80% are cataract operations.” It pointed out that, despite this, the service delivered 4,000 more outpatient visits in 2024 than in 2023, which it achieved achieved through “innovation, efficiency and overwhelming goodwill from the staff to go the extra mile for our patients”.
HDC Morag McDowell said that she is “very concerned that despite some measures having been put in place, there are ongoing risks to patients”. She noted that Waitaha Canterbury district’s unprecedented capacity constraints are not forecast to improve for the foreseeable future.
McDowell recommended that regional leadership at Health New Zealand Te Waipounamu work with the district to undertake an assessment of the mid-to long-term sustainability of the ophthalmology service at Waitaha Canterbury and develop an overall service plan for the ophthalmology service, taking into account the geographical demands of the area, the overall capacity of ophthalmology services within the South Island and allied/technical support needed for any uplift in FTE. An update on the assessment and service plan is to be provided to HDC by Waitaha Canterbury within 12 months of her report.