Corneal research review
A first-in-human clinical study of an allogenic iPSC-derived corneal endothelial cell substitute transplantation for bullous keratopathy
Hirayama M, et al.
Cell Rep Med. 2025 Jan 21;6(1):101847
Review: This is the first in-human study evaluating the safety and efficacy of induced pluripotent stem cell (iPSC)-derived corneal endothelial cell substitutes (CLS001) for treating bullous keratopathy. A 73-year-old male with a history of keratoconus and multiple corneal surgeries received an injection of CLS001 cells into the anterior chamber and was monitored over 12 months. The patient's best-corrected visual acuity improved from 20/1,000 to 20/286 with spectacles and 20/100 with hard contact lenses, postoperatively.
A de novo in-frame deletion in exon 22 of the EP300 gene was identified in the transplanted CLS001 cells. Despite this mutation, no adverse effects were observed.
Comment: Over 12 million patients worldwide are waiting for corneal transplantation, primarily due to the chronic shortage of donors. Corneal endothelial cell substitutes derived from iPSCs do not require a donor cornea and have shown equivalent pump and barrier function to corneal endothelial cells in vitro. This exciting article reports on its first use in the human eye, with modest improvements in visual acuity and corneal oedema.
The report highlights a de novo mutation that was detected despite extensive preoperative whole-genome sequencing and tumourigenicity testing of the master cell bank. The mutation did not originate during the differentiation process but during the expansion culture of the iPSCs. Such random mutations may be unavoidable with the current sensitivity of whole-genome testing. This report on iPSC therapy is encouraging, but risk management of random mutations requires further development.
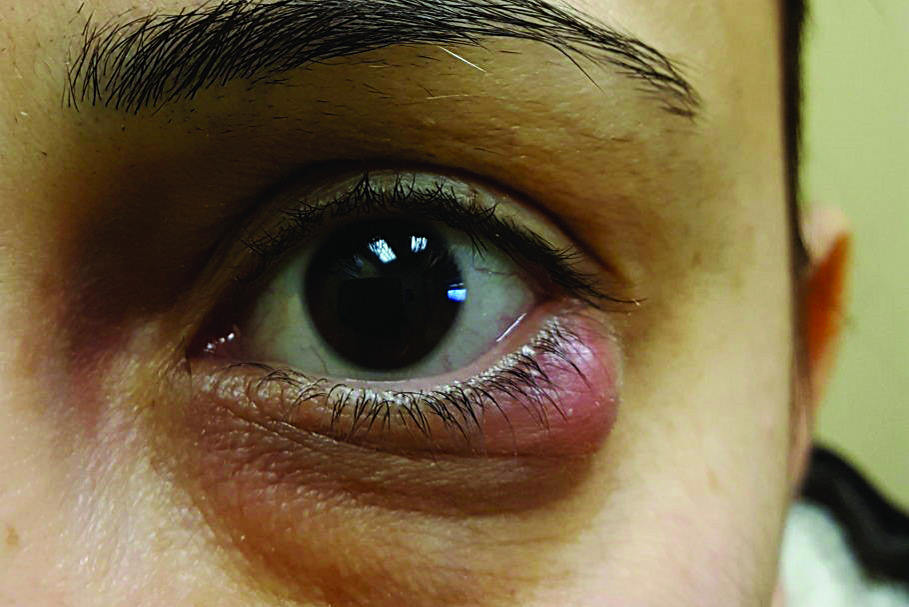
Topical losartan for corneal fibrosis: a case series with densitometry analysis
Burgos-Blasco B, et al.
Cornea. 2024 Dec 13. Epub ahead of print
Review: This case series examined eight eyes of seven patients treated with topical losartan 0.8mg/ml four times a day for six months for corneal scars. The visual acuity of five eyes improved (0.28 ± 0.17 logMAR to 0.17 ± 0.11 logMAR), one eye remained unchanged and the vision of two eyes declined. Although a tendency toward improved corneal densitometry was noted, differences were not statistically significant. No systemic side effects were reported and tolerance was very good or excellent.
Comment: Most of us are familiar with losartan (Cozaar) in treating systemic hypertension. A few case reports have suggested off-label use of topical losartan as an alternative to surgical management of corneal scars. This is based on losartan’s role in inhibiting transforming growth factor-b signalling, a key component in myofibroblast development and scar tissue formation. This is the largest case series to date documenting the effect of topical losartan in treating corneal scarring of different aetiologies, including viral infection and corneal collagen crosslinking.
Although five of eight eyes had improved visual acuity, this was not statistically significant, likely due to the small sample size. Larger randomised studies with longer follow-up are anticipated, as medical therapy for corneal scarring has enormous potential to transform care.
Long-term clinical outcomes and anterior segment OCT findings after artificial endothelial replacement membrane implantation
Fontana L, et al.
Cornea. 2025 Feb 18. Epub ahead of print
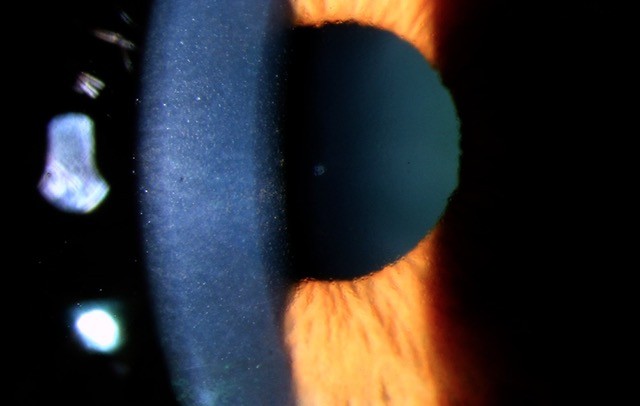
Review: This case series reports long-term outcomes of EndoArt (EyeYon Medical, Israel), a flexible acrylic hydrophilic implant, 6.5mm in diameter, which acts as an artificial fluid barrier against the posterior cornea. Seven patients (mean age 76 years) with prior endothelial keratoplasty (EK) failure (five patients) or bullous keratopathy (two patients) underwent EndoArt implantation and were monitored over 24 months.
Corrected distance visual acuity (CDVA) improved from a mean of 1.32 ± 0.23 logMAR preoperatively to 0.95 ± 0.28 logMAR at 24 months postoperatively (P=0.03). Central corneal thickness (CCT) decreased significantly from 805 ± 131μm preoperatively to 577 ± 90μm postoperatively (P=0.002). Four out of seven patients experienced device detachment, requiring one or more rebubbling procedures.
Comment: This article adds to the growing evidence on the effectiveness of EndoArt in improving corneal transparency and visual acuity for patients with chronic corneal oedema. Current literature reports a high rate of implant detachment, which is a major drawback of this device. However, this can be reduced by using fixating sutures for at least three months. So far, there have been no cases of immune rejection of this implant, making it a potential alternative to traditional EK, especially in complex cases with a high risk of graft rejection or failure.

Dr Bia Kim is a cornea and cataract specialist at Manukau Health Park and Greenlane Clinical Centre and in private practice at Auckland Eye.