Differentiating papilloedema vs pseudopapilloedema in children
Differentiating true papilloedema from pseudopapilloedema in children presenting with bilateral optic disc swelling remains a frequent and complex diagnostic challenge for ophthalmologists and community providers. There is often a degree of associated anxiety not only for the clinician but also the child and their family.
The most diagnostically ambiguous cases are those involving mild papilloedema (Frisen grades 1 and 2), which can closely mimic benign anatomical variants, such as optic disc drusen or anomalous optic discs.
Establishing the correct diagnosis is critically important: failure to identify true papilloedema has potentially life-threatening implications. Conversely, incorrectly diagnosing pseudopapilloedema as papilloedema can subject children to unnecessary, invasive and expensive testing which typically requires sedation or general anaesthesia1.
Furthermore, for a paediatric ophthalmologist receiving community referrals there is a question of the urgency with which the child needs to be seen. A recent study conducted in a large Australian hospital retrospectively reviewed paediatric optic disc swelling referrals (n=410) over a six-year period4. The study found 83.9% (n=344) were pseudopapilloedema and 16.10% (n=66) were true optic disc oedema, representing approximately 1 in 6 children referred for papilloedema. This aligns with the literature, including a prospective study of children who were referred for papilloedema, finding 76% of children were diagnosed as having either pseudopapilloedema or normal optic nerves2.
Papilloedema
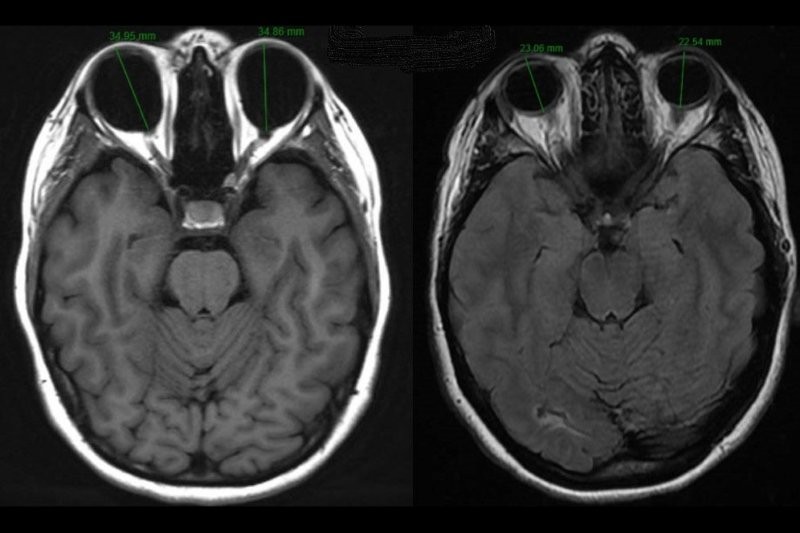
Papilloedema is optic disc oedema that is usually bilateral and occurs due to transmission of raised intracranial pressure to the subarachnoid space surrounding the optic nerve head (Fig 1)1,3. It warrants urgent investigation with neuroimaging +/- lumbar puncture to elucidate the underlying cause. Children with true papilloedema are more likely to present with headaches and visual disturbance and variably tinnitus or vomiting2,4. In one study, 41.57% of patients with pseudopapilloedema had headache vs 86.36% of true papilloedema. All patients with space-occupying lesions had either headache or visual disturbance4.
The most common cause of true papilloedema is idiopathic intracranial hypertension (IIH), followed by space-occupying lesions2,4. IIH is defined as raised intracranial pressure in the absence of a space-occupying lesion or hydrocephalus and normal cerebrospinal fluid5. It is diagnosed with neuroimaging and lumbar puncture5. In children with a space-occupying lesion, neuroimaging and subsequent urgent discussion and referral to neurosurgical services are required.
Pseudopapilloedema
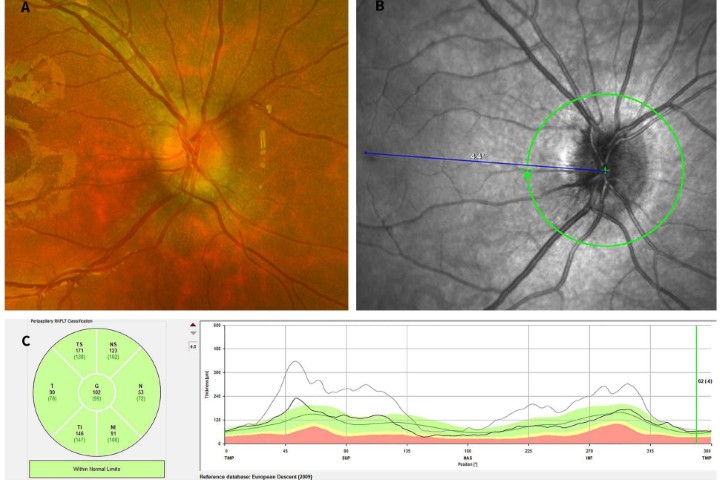
Pseudopapilloedema may be unilateral or bilateral elevation of the optic disc. It is defined by blurring and swelling at the borders of the optic nerve head, secondary to structural anomalies without true oedema of nerve fibre layers (Fig 2)1. Children with pseudopapilloedema are more likely to be asymptomatic, with an absence of visual disturbance; however, they may still report the symptom of a nonspecific headache4. While pseudopapilloedema is a benign condition, it still requires urgent assessment to determine the need for investigation or intervention.

Fig 2: Pseudopapilloedema in an asymptomatic seven-year-old child. A: Optos ultra-widefield fundus photograph demonstrating blurred disc margins. B: En-face Heidelberg OCT image of optic disc. C: Heidelberg optic nerve head image demonstrating PHOMS (white arrow), which remained stable over a six-month period of monitoring. D: Heidelberg OCT retinal nerve fibre measurements demonstrating higher than average thickness which remained stable over a six-month period of monitoring
The most common causes of pseudopapilloedema in the paediatric population are optic disc drusen (ODD), crowded discs – typically in hyperopic children, and tilted discs – typically in myopic children3.
Optic disc drusen are acellular and extracellular deposits that usually calcify over time. Typically, ODD in children are noncalcified and buried within the neural tissue, obscuring their detection with traditional ancillary testing used in adults with ODD6. They typically become superficial and calcified over childhood at the average age of 12 years old7.
Tilted discs are typically bilateral and occur when there is oblique or horizontal orientation of the disc axis and a vertical tilting of the disc, superonasal elevation and a rotated oval or D-shaped disc appearance3,8. Tilted discs can be classified based on their suspected aetiology: congenital, which is characterised by an inferior or inferonasal tilting of the optic disc, or a myopic tilted disc, which is an acquired change related to myopic progression8.
Small, crowded optic discs are typically seen in children with hyperopia due to the shortened axial length. In crowded discs, a normal number of optic nerve axons converge at a small optic disc and course through a narrower than average scleral canal. This may result in indistinct margins and mimic papilloedema9.
No clear consensus exists for the duration of stability of pseudopapilloedema; however, several published studies suggest there should be a minimum period of six months of follow-up without change in optic nerve appearance to meet the criteria for a pseudopapilloedma diagnosis2,4.
It is important to note, true papilloedema may overlay pseudopapilloedema and a clinician must consider papilloedema, even if there have been other findings, such as disc drusen10.
Ophthalmic imaging modalities
When faced with a child with potential optic disc oedema there is a need to choose imaging tools with precision, as often a child’s engagement will be time constrained. While each ophthalmic imaging tool can contribute to differentiating papilloedema from pseudopapilloedema, each has its limitations and no gold standard exists.
There are anatomical features of the optic disc which may help differentiate true papilloedema from pseudopapilloedema. True papilloedema manifests as blurred optic disc margins and, as severity progresses, disc haemorrhages and cotton wool spots11. In pseudopapilloedema there are blurred disc margins, but with an absence of vessel obscuration or disc haemorrhages4.
Often fundoscopy examination of children is challenging, with only glimpses of the fundus and disc seen. Optos ultra-widefield fundus photography can be an invaluable tool to enable careful analysis of optic disc features. It can often be performed in young children with gentle encouragement and utilisation of distraction and play.
Fundus autofluorescence (FAF) can easily be taken at the same time as ultra-widefield imaging and is a useful method for identification of superficial optic disc drusen, which appear as brightly autofluorescing lesions at the optic disc3. However, in younger children it is less sensitive due to the ODD being buried and noncalcified12.
Similar to FAF, B-Scan ultrasonography is a well-established imaging modality in the diagnosis of ODD in adults. On ultrasonography, ODD appear as hyperreflective lesions at the level of the optic disc. However, it has less utility in children due to ODD drusen being non-calcified1.
Fundus fluorescein angiography (FFA) has been investigated by multiple studies7,12,13. In pseudopapilloedema there is either no hyperfluorescence or only nodular staining in ODD. In true papilloedema the FFA demonstrates leakage at the optic nerve. For children, the FFA can be performed using ultra-widefield and oral fluorescein (typically diluted in orange juice and given with a straw to reduce staining of teeth), which avoids the challenge of cannulating a child and the distress this can cause14. However, FFA does not provide a definitive answer, especially in cases of mild papilloedema, with one study finding an accuracy of only 62-69%13.
Arguably, the most informative test in assessing optic nerve swelling is spectral-domain-OCT (SD-OCT), a widely accessible imaging modality in both the ophthalmology and optometrist settings. Increased retinal nerve fibre layer (RNFL) thickness in all four quadrants is highly suggestive of true papilloedema but, in practice, in children is often not found3,6.
In a large study investigating children referred for papilloedema, the most notable difference between children with true papilloedema and pseudopapilloedma was RNFL thickness4. An average RNFL thickness of 154.62 ± 63.76µm was seen with true optic disc oedema, followed by an average thickness of 123.11 ± 22.0µm in optic disc drusen and, lastly, an average thickness of 108.92 ± 13.60µm in children with anomalous discs4. Hypermetropic children have an increased average RNFL thickness compared to emmetropic children, but there is a lack of paediatric normative databases based on age or refractive error14. Serial, interval RNFL measurements provide an objective assessment for monitoring suspected papilloedema patients for whom the diagnosis is not clear.
SD-OCT of the optic nerve head can also be used to assess for ODD, which can be identified as circumscribed, hyporeflective, spheroidal masses fully or partially surrounded by a hyperreflective border, located in front of the lamina cribrosa15.
PHOMS are non-specific optic nerve head structures which can be visualised on OCT; however, they are associated both with papilloedema and pseudopapilloedema and therefore should not be used to differentiate between the two pathologies. En face SD-OCT can also be used to detect peripapillary wrinkles, which are distinctive signs of optic disc oedema. By placing the eye in the adducted position, this may expose folds and peripapillary deformations that may not be evident in primary position16.
Summary
The differentiation between papilloedema and pseudopapilloedema is an important but challenging diagnosis. While true papilloedema has potentially serious implications and must be investigated and treated urgently, pseudopapilloedema requires no intervention. Multiple studies have demonstrated that the large proportion of referrals to ophthalmology services for papilloedema result in a diagnosis of pseudopapilloedema, or normal optic discs.
History taking and clinical examination are the crucial first steps in evaluating a child with suspected optic disc swelling. Those with true papilloedema are often symptomatic with headache, visual disturbance and variably tinnitus and vomiting. In contrast, children with pseudopapilloedema are often asymptomatic and the optic disc appearance may be noted incidentally during routine ophthalmic examination.
Although ophthalmic imaging modalities play a key role in the diagnostic process, part of the difficulty is that no gold standard imaging technique exists for definitively differentiating papilloedema from pseudopapilloedema. Widely available imaging modalities include Optos ultra-widefield fundus photography, fundus autofluorescence and SD-OCT. These three imaging modalities can be used to gain important information and ideally would be included in any referral from the community to ophthalmology services as they can aid in triaging their urgency for suspected papilloedema.
References
- Chang MY, Binenbaum G, Heidary G, Morrison DG, Galvin JA, Trivedi RH, et al. Imaging Methods for Differentiating Pediatric Papilledema from Pseudopapilledema: A Report by the American Academy of Ophthalmology. Ophthalmology. 2020;127(10):1416-23.
- Kovarik JJ, Doshi PN, Collinge JE, Plager DA. Outcome of pediatric patients referred for papilledema. Journal of the American Association for Pediatric Ophthalmology and Strabismus (JAAPOS). 2015;19(4):344-8.
- El-Gendy RS, El-Hamid ASA, Galhom AEA, Hassan NA, Ghoneim EM. Diagnostic dilemma of papilledema and pseudopapilledema. Int Ophthalmol. 2024;44(1):272.
- Li Y, Dai S. Clinical approach for suspected optic disc swelling in children: recommendations based on a six-year review. Clin Exp Optom. 2023;106(7):793-9.
- Standridge SM. Idiopathic intracranial hypertension in children: a review and algorithm. Pediatr Neurol. 2010;43(6):377-90.
- Kaplan AT, Öskan Yalçın S, Güneş Sağer S. Clinical Findings and Optical Coherence Tomography Measurements of Pediatric Patients with Papilledema and Pseudopapilledema. Turk J Ophthalmol. 2023;53(5):294-300.
- Chang MY, Pineles SL. Optic disk drusen in children. Surv Ophthalmol. 2016;61(6):745-58.
- Cohen SY, Vignal-Clermont C, Trinh L, Ohno-Matsui K. Tilted disc syndrome (TDS): New hypotheses for posterior segment complications and their implications in other retinal diseases. Progress in Retinal and Eye Research. 2022;88:101020.
- Chiang J, Wong E, Whatham A, Hennessy M, Kalloniatis M, Zangerl B. The usefulness of multimodal imaging for differentiating pseudopapilloedema and true swelling of the optic nerve head: a review and case series. Clin Exp Optom. 2015;98(1):12-24.
- Tavakoli M, Yan F, Tauscher R. Concomitant optic disk drusen and papilledema due to idiopathic intracranial hypertension in a pediatric cohort. J aapos. 2024;28(1):103806.
- Frisén L. Swelling of the Optic Nerve Head: A Backstage View of a Staging Scheme. J Neuroophthalmol. 2017;37(1):3-6.
- Chang MY, Velez FG, Demer JL, Bonelli L, Quiros PA, Arnold AC, et al. Accuracy of Diagnostic Imaging Modalities for Classifying Pediatric Eyes as Papilledema Versus Pseudopapilledema. Ophthalmology. 2017;124(12):1839-48.
- Elhusseiny AM, Fong JW, Hsu C, Grigorian F, Grigorian AP, Soliman MK, et al. Oral Fluorescein Angiography for the Diagnosis of Papilledema Versus Pseudopapilledema in Children. American Journal of Ophthalmology. 2023;245:8-13.
- Marmoy OR, Henderson RH, Ooi K. Recommended protocol for performing oral fundus fluorescein angiography (FFA) in children. Eye (Lond). 2022;36(1):234-6.
- Malmqvist L, Bursztyn L, Costello F, Digre K, Fraser JA, Fraser C, et al. The Optic Disc Drusen Studies Consortium Recommendations for Diagnosis of Optic Disc Drusen Using Optical Coherence Tomography. J Neuroophthalmol. 2018;38(3):299-307.
- Sibony PA, Kupersmith MJ, Kardon RH. Optical Coherence Tomography Neuro-Toolbox for the Diagnosis and Management of Papilledema, Optic Disc Edema, and Pseudopapilledema. J Neuroophthalmol. 2021;41(1):77-92.

Dr Martin Wasik is a neuro-ophthalmologist working at Greenlane Clinical Centre

Dr Helen Kearns is a non-training ophthalmology registrar at Greenlane Clinical Centre