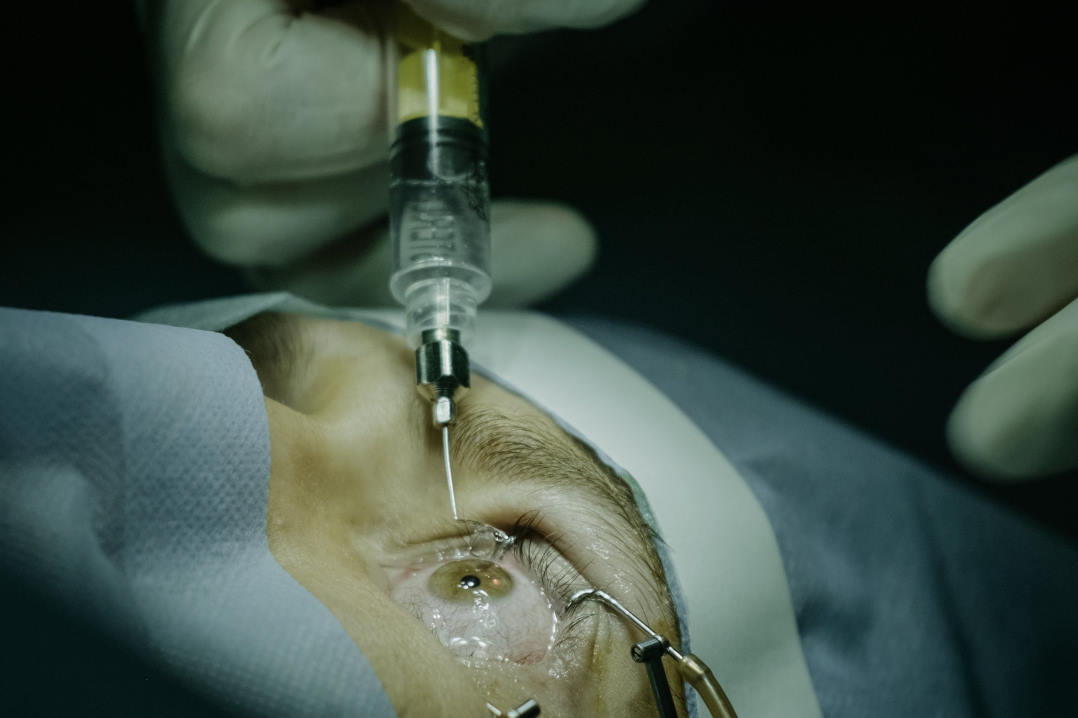
Keratoplasty infections jeopardise grafts
The authors of a University of Auckland study say keratitis after corneal transplantation remains an important threat to graft survival, with infection episodes markedly increasing the likelihood of graft failure. The findings come from a 12-year review of all keratoplasties performed in Auckland, published in International Ophthalmology and led by PhD candidate Natalie Allen, with co-authors A/Prof Rachael Niederer, Drs Akilesh Gokul and Jie Zhang and Professor Charles McGhee.
The team analysed 1,184 keratoplasties performed between 2010 and 2022, representing 974 patients, to evaluate keratitis risk in Auckland’s mild, humid, subtropical climate, alongside risk modifiers, microbial resistance and graft outcomes.
The authors reported a cumulative keratitis incidence of 2.4% at one year and 6% at five years, noting this steady rise underscored the need for long-term vigilance. They said most infections were bacterial, with viral, fungal, parasitic and autoimmune causes also identified. Increasing age, Asian ethnicity and poor treatment compliance significantly elevated risk. Graft type was also influential: endothelial keratoplasty carried the lowest keratitis rate at 2.1%, while penetrating keratoplasty reached 7.8%. Although anterior lamellar keratoplasty showed a 7.9% rate, the authors said this was not statistically significant. They reported that any episode of keratitis more than doubled the risk of graft failure.
Given concerns that pandemic-era disruptions might worsen outcomes, the authors examined Covid-period grafts and found no increased keratitis incidence, concluding that reduced in-person care did not translate into higher infection risk. They added that antibiotic resistance remained low and emphasised treatment compliance and graft selection as the only modifiable risk factors.