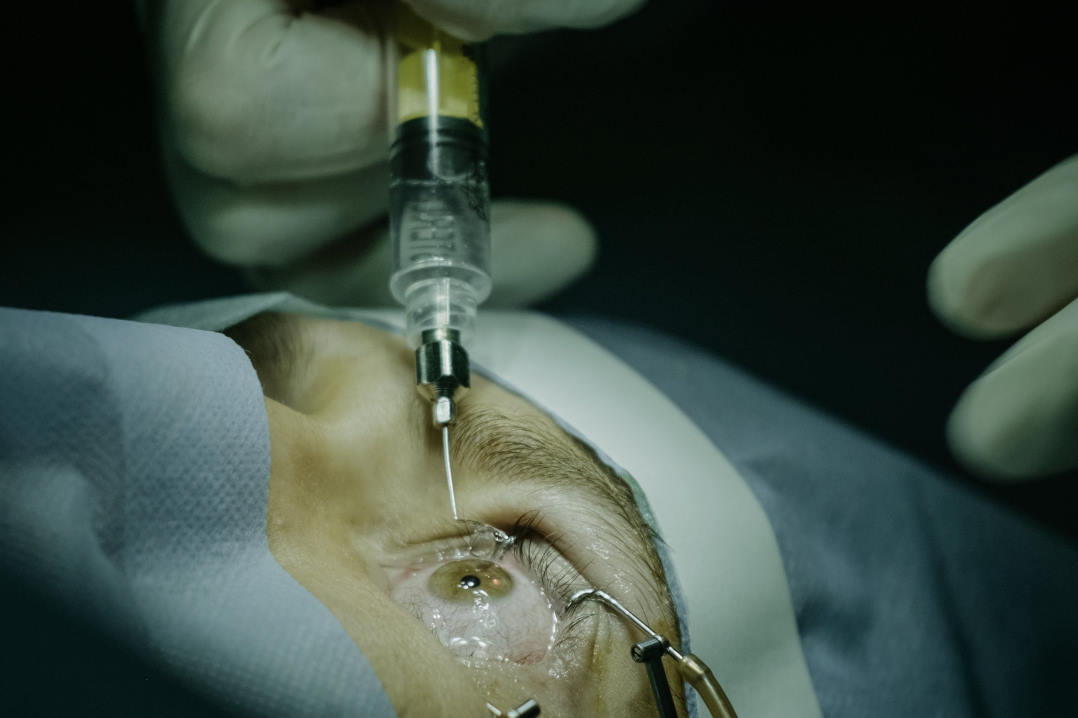
NZ survey exposes gaps in scleral shell care
Researchers at the University of Auckland found “significant inconsistencies” in the way clinicians manage patients with blind disfigured eyes, specifically regarding the provision and care of custom scleral-shell prostheses.
In the first national study of its kind, the team of Associate Professors Robert Jacobs and Stuti Misra, Dr Brian Sloan and ocular prosthetists Janice Yeoman and Dr Keith Pine surveyed 140 optometrists, 50 ophthalmologists and eight ocular prosthetists about their understanding of indications, maintenance and complications related to scleral-shell wear. The data showed patients with non-functional disfigured eyes (NFDEs) were far less likely to receive an ocular prosthesis than those with anophthalmia (~30% vs >90%, respectively).
Responses among optometrists and ophthalmologists about which clinical presentations were suitable for shell wear were inconsistent, but both groups were concerned about shells’ risks of keratitis and discomfort. Ocular prosthetists reviewed significantly more prosthetic-eye wearers than scleral-shell wearers annually (184 ± 113 prosthetic eye wearers/year vs 17.3 ± 20.6 scleral shell wearers/year) and reported never assessing prosthetic contact lens patients.
Most optometrists (71%) and ophthalmologists (68%) recommended prosthetic contact lens fitting initially to patients with clinically stable NFDEs who were concerned about their appearance. Fewer suggested scleral shells, or other options first (including eye removal with subsequent prosthetic eye wear). For shell wearers, optometrists and prosthetists typically advised daily cleaning and no overnight wear, while ophthalmologists offered mixed guidance.
The study identified a lack of coordination between disciplines, said researchers. This is compounded by ocular prosthetists lacking scope to manage ocular health beyond shell fabrication and fitting, while many optometrists and ophthalmologists had little practical experience with shells.
As NFDEs can vary widely in their clinical presentation, optometrists and ophthalmologists need clear guidelines to identify suitable shell candidates, concluded authors. “Information on best-practice maintenance and wear protocols is also required to support long-term complication-free shell wear.”