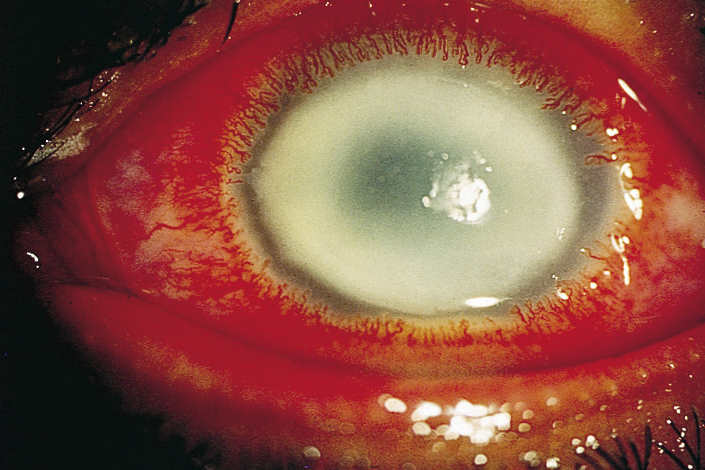
Outcome insights for Acanthamoeba keratitis?
A retrospective audit of Moorfield’s medical records over 20 years, published in the British Journal of Ophthalmology, has provided risk factor insights for poor outcomes and severe inflammatory complications (SICs) for patients with Acanthamoeba keratitis.
Of 194 patients reviewed, 93 had poor outcomes - defined as corneal perforation, keratoplasty, other ocular surgeries, duration of antiamoebic therapy (AAT) of 10.5 months or more and a final visual acuity of 20/80 or less. SICs included scleritis and/or corneal stromal ring infiltrates. Patients were found to be at higher risk of poor outcomes if they were older than 34 and had used corticosteroids before AAT; more advanced disease was also a risk factor; and SICs development was significantly associated with herpes simplex virus (HSV) keratitis treatment before AAT.
According to the authors, the association of both poor outcomes and SICS with older age may be related to impoverished host defences, while delayed treatment and previous treatment with steroids, may predispose the patient to an increase in the quantity and distribution of Acanthamoeba, making the disease more difficult to treat. Finally, the increased rate of SICs in eyes previously treated for HSV keratitis may be due to an altered immune response of the cornea after treatment with acyclovir, wrote the authors. “This analysis of risk factors for bad outcomes and SICs adds to the existing evidence that delayed diagnosis, misdiagnosis of AK as HSV keratitis and topical corticosteroid use before AAT are avoidable risk factors for bad outcomes.”