RANZCO 2025 insight, empathy and innovation
The 2025 RANZCO Annual Scientific Congress brought the ophthalmology community together at the Melbourne Convention and Exhibition Centre. Set against the backdrop of a city known for its cultural delights and incredible international cuisine and coffee, it hosted more than 2,800 delegates and 11 phenomenal keynote speakers who came from all corners of the globe and shared some excellent clinical pearls.
The congress opened with a deeply beautiful and touching presentation by Rachel Callander, a University of Otago alumna. Her talk, ‘The power of language we use in patient-centred ophthalmic care,’ was framed through the lens of her own journey through the medical system as a mother to Evie, her daughter with trisomy 18. She graciously reminded us to look for beauty in the brokenness and in discarded places – aspects we often overlook when we are caught up in the daily motions of service delivery. It was a powerful, grounding start that centred our focus on the human element of our practice.
Deep dive into ocular oncology

Dr Sandra Staffieri
Having only recently been awarded my PhD in ocular oncology, I was personally delighted with the keynote lineup’s emphasis on adult and paediatric ocular tumours, specifically uveal melanoma and retinoblastoma. Dr Sandra Staffieri, a clinical and research orthoptist from The Royal Children’s Hospital Melbourne with 40 years of paediatric ophthalmology experience and who trained with none other than Professor Fred Hollows himself, took us through her experience in her service on referrals and diagnosis of retinoblastoma in the Fred Hollows Lecture. Her key message was a stark but hopeful reminder: “Retinoblastoma awareness is the difference between being sighted and sightless.” She emphasised this is one of the most survivable paediatric cancers, provided diagnosis is early and follow-up is robust.
Joining us from the University College London Institute of Ophthalmology and Moorfields Eye Hospital, Professor Mandeep Sagoo delved into his subspecialties of adult and paediatric eye tumours. Across a number of presentations, he delivered the latest updates in uveal melanoma diagnosis, clinical controversies in retinoblastoma treatment – especially in moderate to larger-sized tumours, as well as the plethora of imaging modalities in monitoring, diagnosing and assessing treatment outcomes/recurrences of various ocular tumours. I was fascinated by his efforts in digitalising the ocular prosthetic-fitting experience, which was a perfect example of the seamless incorporation of artificial intelligence (AI) in ophthalmic medicine.
The AI and technology revolution
The technology theme continued with Dr Clare Bailey from Bristol Eye Hospital. She delivered a compelling talk on using AI to quantify fluid on OCT scans in retina clinics and detect geographic atrophy in those with macular degeneration. She also presented on a number of pivotal moments in her hospital’s retinal treatment unit, especially during and after the Covid-19 pandemic era. Specifically, she described the NHS’ efforts in moving towards a unified electronic medical record for patients with retinal disorders and the development of service delivery via a hub-and-spoke model. The latter saw satellite clinics set up in places such as a supermarket car park (which proved popular due to the ample free parking!), as well as the move of the Bristol Eye Hospital Assessment Service to a local shopping mall for easier community access.
Dr Radhika Tandon, from All India Institute of Medical Sciences, New Delhi, also discussed AI-assisted algorithms that facilitate early detection of corneal diseases and guide referral pathways and risk stratification for corneal conditions. Her insights into how precision medicine will shape the future of global corneal care were truly forward-thinking.
Surgical and clinical updates
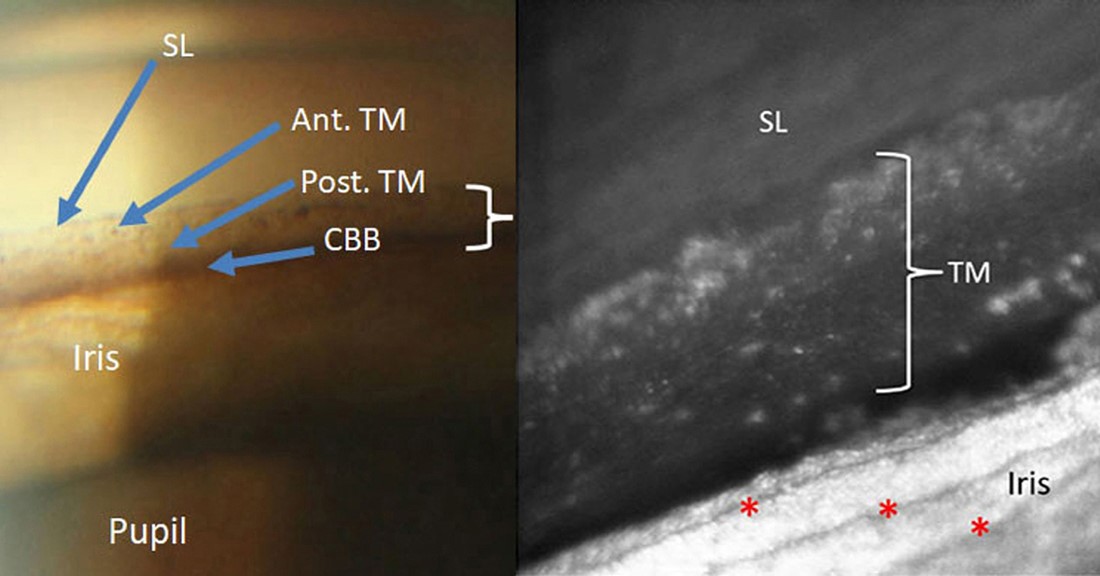
Moorfields’ Professor Gus Gazzard challenged us to consider whether interventional glaucoma is “myth, magic, or monster”. He highlighted the evolving training landscape for future surgeons, where the classic trabeculectomy may no longer be the first-line treatment given the rise of minimally invasive glaucoma surgery, minimally invasive bleb surgery and drainage tubes.
The uveitis update on ocular toxoplasmosis and syphilitic uveitis by Professor Daniel Vitor Vasconcelos-Santos, from UFMG School of Medicine, Brazil, was fantastic. Using slides from multimodal imaging to present the data, he reminded us that syphilis is re-emerging globally and stressed the importance of using serology testing to distinguish between past and active infections.

Prof Anders Behndig
Next, Professor Anders Behndig, Umeå University, Sweden, took us through the recent developments in cataract surgery, which is still the most common operation in the world. He detailed various techniques and ways to optimise tools of the trade using biometry calculations and choices of lens and reminded us that multifocal and extended depth-of-focus (EDOF) intraocular lenses, while controversial to some, are still important components of the surgical armamentarium. I especially enjoyed how he brought us back to the basics of how multifocal and EDOF lenses were developed and the physics behind them.
Celebrating home-grown excellence
The named lectures this year were memorable, featuring leaders in their fields from Australia and New Zealand. The Dame Ida Mann Memorial Lecture came courtesy of Associate Professor Andrea Vincent, regarded as New Zealand’s first molecular ophthalmologist clinician-scientist, who took us on a mesmerising journey through Polynesia. She unpacked the genetic basis of eye diseases in Māori and Pasifika, tracing many conditions back to whakapapa lines associated with the traditions of the seven great waka, which I found particularly interesting.
The University of Adelaide’s Professor Dinesh Selva then delivered an enlightening talk on endoscopic orbital surgery for the Norman McAlister Gregg Lecture. Having recently observed my first endonasal orbital decompression, I could fully appreciate his insights into navigating the complex anatomy of the orbit, through the orbital fat, extraocular musculature and crucial neurovascular structures.
For the Council Lecture, Professor Celia Chen, Flinders University, took us on a deep dive into the management of central retinal artery occlusion, a condition often causing profound and permanent visual loss but, more importantly, often associated with undiagnosed risk factors for other major cerebrovascular events. She challenged the current evidence, noting that, while the international Assessment Group for Interventional Lysis in Eye study showed promise for thrombolysis with visual recovery using intra-arterial and intravenous thrombolysis treatment when compared with non-thrombolytic treatments, we still need sufficiently powered randomised controlled trials to confirm the efficacy of these treatments.
Mysteries and mentorship
Two concurrent sessions stood out for me. The first was the Medical Retinal Mysteries session chaired by Westmead Hospital and Macquarie University’s Professor Adrian Fung, the founding editor of the Westmead Eye Manual that many ophthalmology trainees refer to for our clinical practice. It was so well attended there were as many standing as were seated, all to join the vibrant discussions around white dot syndromes, retinal toxicity presentations and a plethora of inherited, traumatic and nutritional retinal diseases. It was fast-paced, full of pearls and delivered with punchlines and well-timed humour, making it all the more memorable.

Prof Dame Helen Danesh-Meyer, Dr Liz Unsull and author Dr Joevy Lim
The second stand out was the Women in Ophthalmology luncheon, hosted by Bayer, that also attracted a full house. We warmly congratulated Professor Dame Helen Danesh-Meyer DZNM, the Sir William and Lady Stevenson Chair in Ophthalmology and head of the Academic Neuro-Ophthalmology and Glaucoma Research Unit at the New Zealand National Eye Centre, on her seven-year tenure as the RANZCO Women in Ophthalmology chair. We also welcomed Associate Professor Penny Allen, head of bionic eye/vitreoretinal research at Centre of Eye Research Australia and head of the Vitreoretinal Surgical Unit at the Royal Victorian Eye and Ear Hospital. The guest speaker, Dr Lily Vrtik, specialist plastic and reconstructive surgeon from Brisbane, delivered an incredible talk that both highlighted and challenged our current understanding of what it is like to be a female surgeon now. She shared her lived experience of perceptions and truths while serving her presidency for the Australasian Society of Aesthetic Plastic Surgeons. Her experiences reminded me of the ‘Let Them Theory’, in the book of the same name by author Mel Robbins, an invaluable mindset in one’s professional and personal life. (Basically, Roberts tells us to stop trying to manage others and simply let people be. In doing so, we protect our energy and create healthier, calmer relationships).
A personal celebration
This conference was extra special as I witnessed the graduation of a number of close friends and colleagues, mentors and supervisors with whom I had the pleasure of working. A special mention to Drs Bia Kim, Ellen Tyler, Lucy Lu and Tiffany Ma, who are now working as consultant ophthalmologists with subspecialty interests in cornea, glaucoma, uveitis and medical retina, and paediatrics, respectively.
No ophthalmic conference can succeed without the generous support of our industry sponsors and boy did they deliver this year! With 91 industry exhibitors and 109 stands to visit at the expo, the delegates were absolutely spoilt with the latest tech and developments. I bade Melbourne farewell, having replenished my cup with the latest academic and clinical advancements, fellowship with friends, colleagues and mentors, and a soul nourished by Gelato Messina and the famous Lune pain au chocolat.
I cannot wait to see everyone again at this year’s congress, proudly held on my home ground of Auckland, from 6–9 November. I also warmly extend an invite to the biennial Women in Vision NZ Conference on Waiheke Island on 4–5 November. See you there!
Dr Joevy Lim is a second year RANZCO trainee based in Auckland. She is a recipient of the prestigious Health Research Council Clinical Research Training Fellowship for ‘A contemporary appraisal on ocular melanoma in New Zealand (Aotearoa)’, for which she was awarded a PhD without corrections.