RANZCO: Advances in Ophthalmology
September’s Royal Australian and New Zealand College of Ophthalmologists (RANZCO) event highlighted the ophthalmological advances anticipated in the next five years, including improved sustainability, genetic and virtual screening and artificial intelligence (AI) – all intended to improve disease prevention, health equity, sight and quality of life.
The Hon Christopher Pyne, chairman of Vision2020 Australia, said 90% of vision loss is avoidable and Australians are currently experiencing consult delays of up to nine months, when Vision2020 Australia is advocating for review within 90 days. He highlighted the need to close the gap in health equity with Indigenous populations, rural and remote regions, as well as other vulnerable communities such as aged care. The aim of this event was to open our eyes to routes to achieving these outcomes.
Sustainability and bioengineering
Dr Jesse Gale started by suggesting ways RANZCO could address sustainability and climate change. Most carbon emissions from eyecare are due to heating, lighting, powering equipment, procurement and transport of patients and staff, he said. He suggested starting with reusing instruments, organising injection clinics closer to home and making a conscious effort to reduce unnecessary clinic visits. Dr Jo Richards from Perth’s Western Eye followed, highlighting the wastefulness of over-prescribed antibiotics, which she said account for AU$1.2million per year of inappropriate chloramphenicol use, and double that amount for ofloxacin. She referenced multiple studies showing the use of iodine pre-operatively plus intracameral cefuroxime was enough. In fact, post-operative antibiotics such as chloramphenicol caused no significant reduction in endophthalmitis rates, resulting in five teaching hospitals in Australia having discontinued their use.
Discussing the advances in corneal stem cells and bioengineered corneas, Professor Stephanie Watson showed the progress being made with simple limbal epithelial transplantation (SLET) and cultivated limbal stem cells. Her team is achieving success rates of 63% with a contact lens technique and will further implement nanotechnology. Professor Gerard Sutton highlighted the global issue with corneal transplants, with only 1 in 70 among those needing corneal transplants receiving them, due to access issues. He helped create BIENCO (BIo ENgineered COrnea), a consortium of world-class organisations which have come together to create a full-thickness bioengineered corneal graft, as well as specific corneal layers. This research has created an electro-compacted collagen stromal sheet with live printed cells, which will change the way we perform corneal transplants, bypassing the difficulties of access to tissue altogether.

Professor Stephanie Watson
Tackling genetic disorders and virtual screening
The University of Sydney’s Professor Robyn Jamieson, alongside the University of Auckland’s Associate Professor Andrea Vincent and the Australian National University’s Associate Professor Riccardo Natoli, explored advances in gene therapy. We can now have a genomic diagnosis in 70-80% of inherited retinal dystrophies, although we don’t always know the consequences of results such as variants of uncertain significance. The most advanced gene therapy exists for RPE65-related dystrophies, which are targeted by Luxturna (voretigene neparvovec-rzyl), with other therapies on the horizon. Polygenic and complex diseases such as glaucoma and age-related macular degeneration (AMD) are now also being targeted. Research shows gene therapy can reprogram Müller glial cells into retinal pigment epithelial cells and retinal ganglion cells, rescuing 70% of retinal ganglion cells. We can also consider gene silencing, using RNA to deactivate the production of incorrect or faulty proteins in ocular diseases. This technology is still very new and there is much about genetic eye disorders we don’t know. This was highlighted by A/Prof Vincent, whose description of certain antioxidants being beneficial to some but harmful to others is a reminder that a personalised approach is still required.

Professor Robyn Jamieson
Melbourne University’s Professor Keith Martin and Dr George Kong, plus University of Sydney’s Professor Nick Strouthidis, explored the advances in virtual consults for complex long-term conditions such as AMD and glaucoma. With an ageing population, demand for care of these conditions is expected to increase 44% over the next 20 years. Current devices such as the Melbourne Rapid Fields (MRF), Eyecatcher from the UK and virtual reality goggles, aim to increase at-home visual fields testing, which has been shown to increase detection of progression and earlier treatment of glaucoma. While at Moorfields, Prof Strouthidis was able to partake in the development of a virtual glaucoma clinic using electronic patient records and imaging clinics, of which some were remote. Although some negative feedback was given – such as patients preferring to see doctors – in general this was well received with great results, including increased discharge rates and increased clinic capacity.
Artificial intelligence and machine learning
Healthcare practitioners have for years been concerned about their future irrelevance with advances in AI and robotics. Wellington’s Dr Cam Loveridge-Easther discussed AI in health and how internet-based software to track patient outcomes is already relevant to ‘big data’. Currently, there are 46 US Food and Drug Administration-approved algorithms that are mostly image-based within the medical field. Melbourne’s Drs Andrew Crawford and Zachary Tan said the biggest AI concern is a lack of regulation and evidence showing machines can perpetuate bias. One example was when an algorithm was translated to a different population, they found it missed 25% of diabetic retinopathy diagnoses. Clearly, models need to adapt to specific populations and this technology must be rigorously tested before real-world application.
Chief medical officer of medical robotics company Preceyes BV, Professor Marc de Smet demonstrated using robotics to perform surgery reduced drift and tremors and significantly reduced complications, despite increasing surgical time. Professor David Mackey from the University of Western Australia then introduced us to Perth’s driverless Intellibus (which we will get to visit during RANZCO Perth 2023), and Waymo (formerly Google’s) driverless cars, which have driven blind passengers. I found it astonishing that despite the proven safety, we still don’t have this service available! However, as Prof Mackey pointed out, there is currently no legislation for driverless cars.
Conclusion
This event was inspirational and I am very much looking forward to these cutting-edge advances becoming reality. The future is here, and I can envisage a more sustainable, equitable and efficient provision of healthcare, keeping patient safety, convenience and quality of life at the forefront.

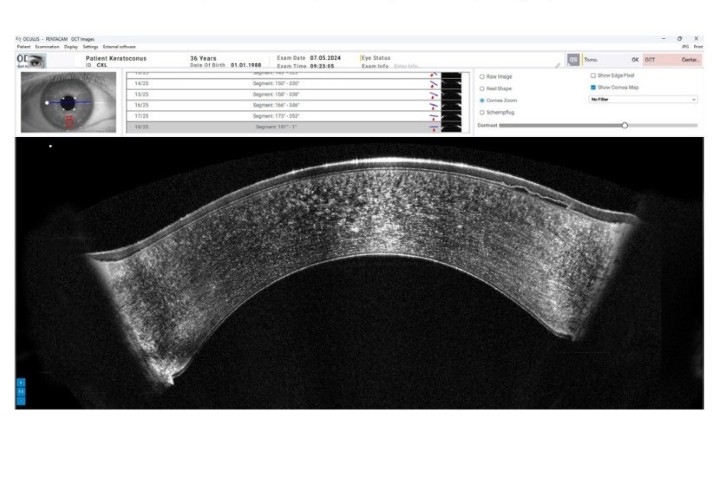
Dr Lize Angelo is an HRC clinical research fellow pursuing a PhD in diagnosing and treating keratoconus, including aspects of equity of access to services in Aotearoa, in the University of Auckland’s ophthalmology department, headed by Professor Charles McGhee.