The resurgence of the scleral lens
Scleral contact lenses have been prescribed to manage ocular surface disease and vision since the 1890s. In 2010, rigid lenses made up just 0.7% of all contact lens (CL) fits, prompting many key opinion leaders to predict the lenses’ demise. However, rigid lenses have seen a dramatic resurgence, now accounting for 21% of all CL fits. Whereas scleral CL fits, which had become virtually non-existent, represented 23% of all rigid CL fittings in 2024 – a remarkable turnaround1.
One reason for scleral lenses’ renaissance is while they were once reserved exclusively for individuals with advanced keratoconus, they are now commonly prescribed to address mild and moderate cases. Their growing popularity can also be attributed to increased comfort by vaulting the cornea, stable refractive correction, reduced dryness symptoms and greater overall tolerance. The rising prescription rates have paralleled a surge in related peer-reviewed publications2.
According to recent findings, scleral lenses are increasingly being used as the first-line treatment for corneal irregularities3.
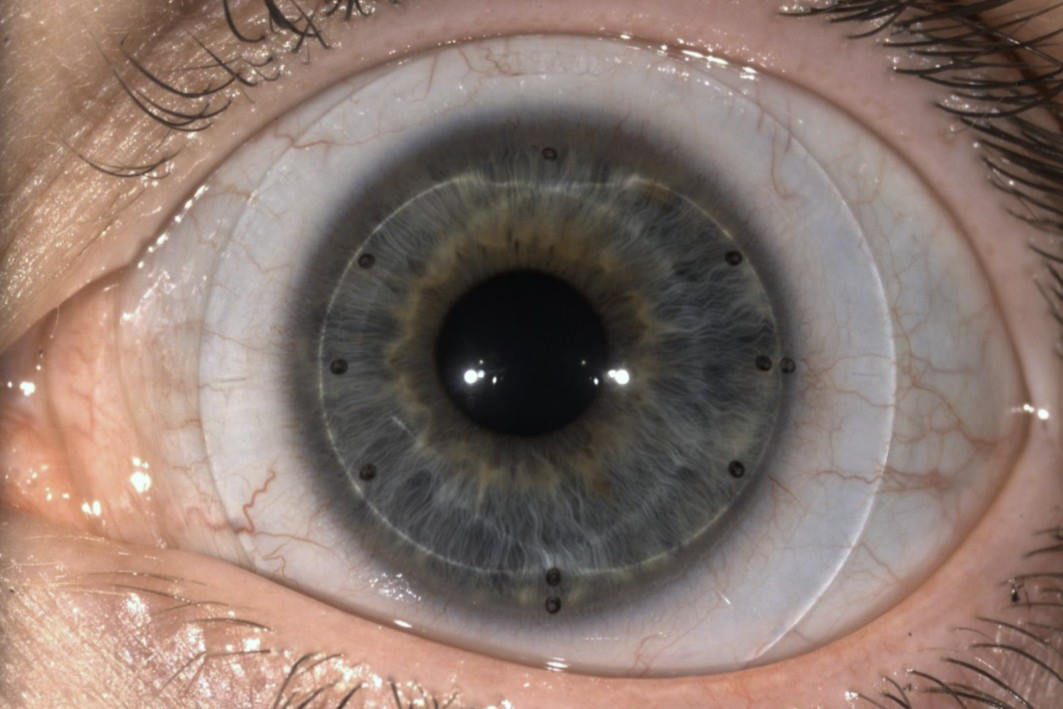
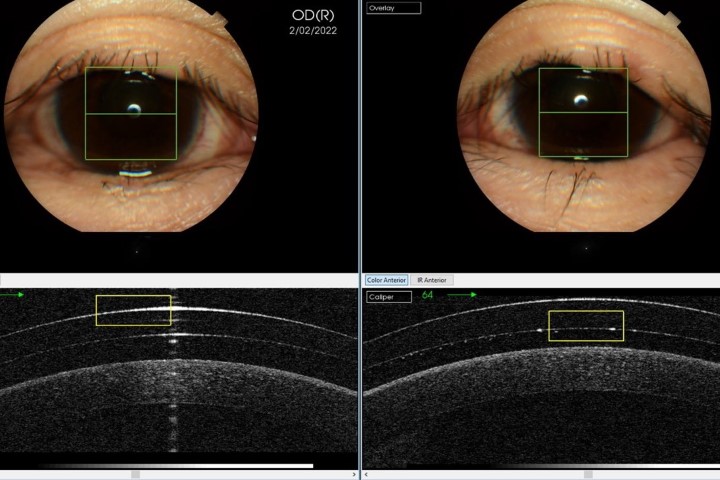
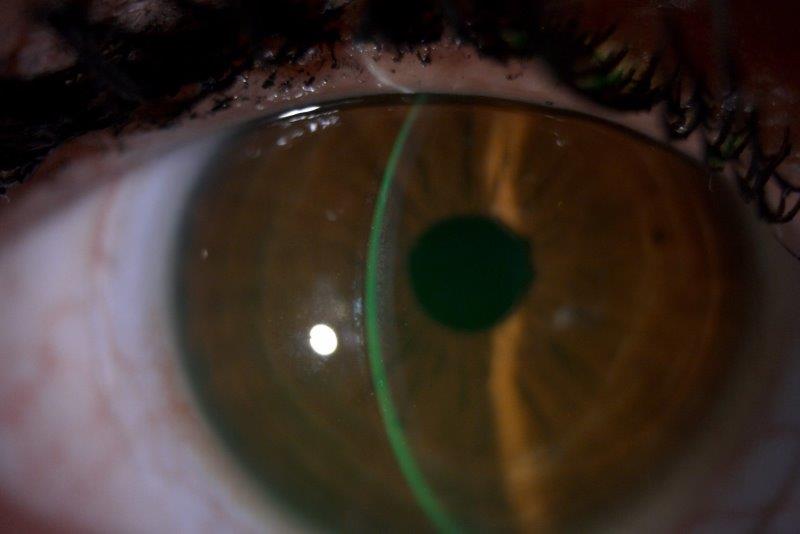
Advancements in lathing techniques and high oxygen-permeable materials have enabled the manufacture of complex, customisable lenses without compromising corneal health (Fig1). Furthermore, developments in ophthalmic instrumentation have simplified the scleral lens fitting procedure for practitioners and enhanced the precision of fit. Accurate estimates of scleral curvature and sagittal depth of the landing zone have led to an increase in successfully fitting the first lens. Increased accessibility to technology, such as anterior OCT, has facilitated non-invasive in-vivo examination of scleral lens fit on the conjunctiva and cornea, improving fit precision and troubleshooting capabilities.
Compared to corneal rigid lenses, scleral lenses offer improved vision, comfort and retention in keratoconus patients4. Individuals refitted from corneal to scleral lenses often report significantly higher satisfaction4. The improved comfort is a result of the lens not landing on the highly sensitive corneal nerves, no eyelid margin interaction, plus a reduction in dry eye symptoms. The sealed scleral lens protects the cornea with a reservoir of preservative-free lubricants/saline, providing relief even in windy or low-humidity environments5.
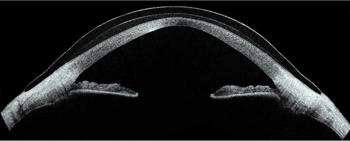
Fig.1: Scleral contact lens
Keratoconus: a complex condition
Despite the increasing pace of innovation in vision care, there are many conditions that do not have effective therapies, keratoconus being one example. Characterised by progressive thinning and distortion of the cornea (Fig 2), the irregular cornea introduces higher-order aberrations (HOAs), resulting in significant visual impairment6. It predominantly affects young individuals, with an estimated prevalence of 1 in 84 among Australian 20-year-olds (85.7% of study participants being White)7. A result of this early onset is a worse quality of life than with retinal diseases such as age-related macular degeneration and diabetic macular oedema8.
Traditional glasses or CLs often fall short in improving vision for these individuals due to the presence of HOAs induced by the irregular cornea.

Fig.2: Keratoconus
What are HOAs?
Most of us are familiar with myopia, hyperopia and astigmatism. These are lower-order aberrations and they're easily corrected with glasses or standard CLs. HOAs, such as coma, trefoil and spherical aberration, are more complex and subtle imperfections in the eye's optics. They cause visual degradation and symptoms, such as glare, halos, ghosting and poor contrast, especially in low-light conditions.
Rigid CLs, such as scleral lenses, can help reduce HOAs by providing a regular anterior optical interface to focus incoming light over the irregular cornea. Some HOAs can be minimised by scleral lenses, but others remain uncorrected, leading to visual degradation9. These residual aberrations will often be in the opposite direction partly due to the compensatory aberration profile of the posterior cornea10.
These residual aberrations can be measured with wavefront aberrometry, which maps how light traverses the eye. Because scleral lenses have minimal movement once fitted, this stable system allows for correction of residual HOAs by applying an inverse aberration profile to the front surface of the lens.
Longitudinal spherical aberration scleral lenses
Negative longitudinal spherical aberration (LSA) lenses are a type of aberration-control scleral lens designed to reduce residual HOAs through targeted optical control. They utilise the natural inferior temporal decentration of the scleral lens due to gravity and the higher nasal sclera elevation to reduce both coma and spherical aberration (Fig 3).

Fig.3: Scleral lens decentration
It’s a simple design targeting the two visually significant HOAs of spherical aberration and coma (Fig 4). Any practitioner can prescribe this scleral contact lens as it does not require the use of an aberrometer (although access to one is beneficial), there is no additional cost to manufacture the lens and the scleral lens does not need to be rotationally stable.
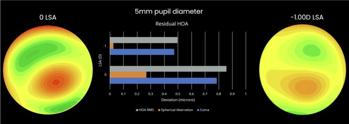
Fig.4: Residual aberrations
Custom aberration-controlled scleral lenses
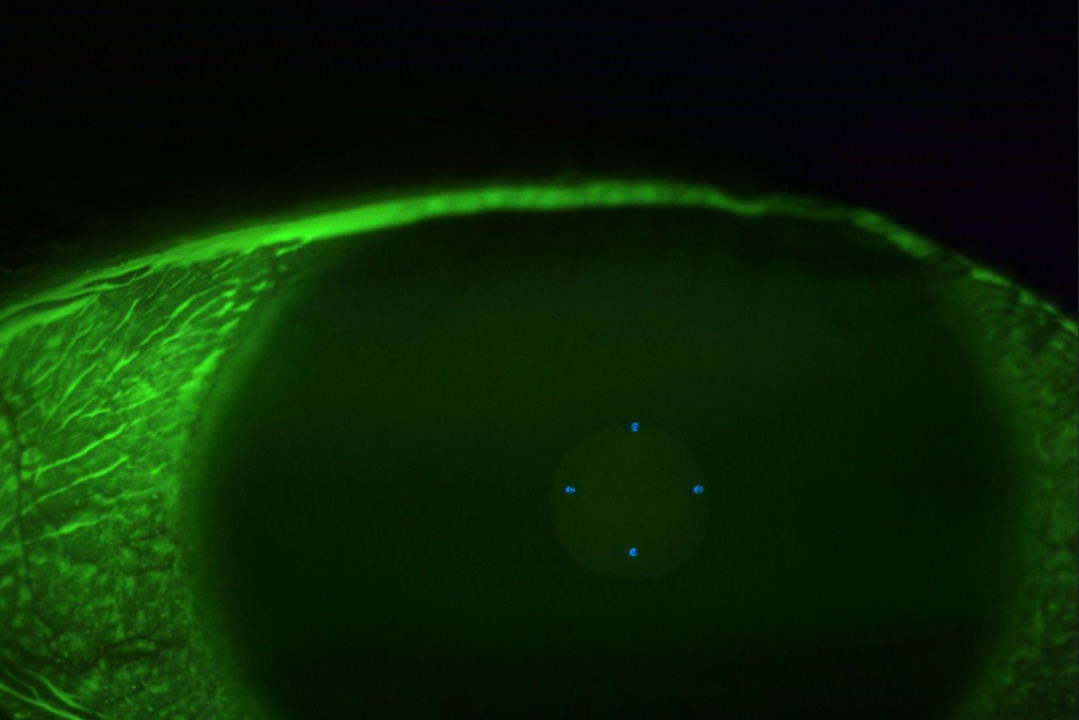
The latest development is completely customisable wavefront-guided scleral lenses. This form of correction is targeted to the patient’s residual aberration profile and requires the reliable determination of specific HOA terms. To create these lenses, wavefront aberrometry is performed to capture the aberrations of the individual wearing a marked conventional scleral lens (Fig 5 see pic at the top). The inverse of this wavefront is then applied to counteract the residual aberration through destructive interference on the front surface of a new lens. Recent studies have shown the majority of patients prefer these lenses to conventional scleral lenses11.
This level of precision doesn’t come easily. Firstly, the completely customisable wavefront-guided scleral lenses must be rotationally stable, with limited movement. It also costs more than a conventional scleral lens, requires a specialised aberrometer and typically requires more chair time. But, for the right patient, the benefits far outweigh the hurdles.
As technology improves and becomes more accessible, fully customised wavefront-guided scleral lenses will play a growing role in eyecare. For patients with complex visual needs, the future is aberration-control scleral lenses.
References
- Efron N, Woods CA and Morgan PB. (2025). Quarter of a century of contact lens prescribing trends in Australia (2000–2024). Clinical and Experimental Optometry, 108(2), 123–134. https://doi.org/10.1080/08164622.2025.2451346
- Woods C, Efron, N, Morgan P. (2020). International Contact Lens Prescribing Survey Consortium. Are eye-care practitioners fitting scleral contact lenses? Clin Exp Optom, 103(4), 499–453. https://doi.org/10.1111/cxo.13105
- Shorter E, Fogt J, Nau C, Harthan J, Nau A, Schornack M. (2023). Prescription Habits of Scleral Lenses for the Management of Corneal Irregularity and Ocular Surface Disease Among Scleral Lens Practitioners. Eye Contact Lens, 49(2), 46–50. https://doi.org/10.1097/ICL.0000000000000963\
- Bergmanson JPG, Walker MK, Johnson LA. (2016). Assessing Scleral Contact Lens Satisfaction in a Keratoconus Population. Optometry and Vision Science, 93(8), 855–860. https://doi.org/10.1097/OPX.0000000000000882
- Bavinger JC, DeLoss K, Mian S I. (2015). Scleral lens use in dry eye syndrome: Current Opinion in Ophthalmology, 26(4), 319–324. https://doi.org/10.1097/ICU.0000000000000171
- Maharana P, Dubey A, Jhanji V, Sharma N, Das S, Vajpayee, R. (2016). Management of advanced corneal ectasias. Br J Ophthalmol, 100(1), 34–40.
- Chan E, Chong EW, Lingham G, Stevenson L J, Sanfilippo PG, Hewitt AW, Mackey DA, Yazar S. (2021). Prevalence of Keratoconus Based on Scheimpflug Imaging: The Raine Study. Ophthalmology, 128(4), 515–521. https://doi.org/10.1016/j.ophtha.2020.08.020
- Kandel H, Nguyen V, Piermarocchi S, Ceklic L, Teo K, Arnalich‐Montiel F, Miotto S, Daien V, Gillies MC, Watson SL. (2022). Quality of life impact of eye diseases: A Save Sight Registries study. Clinical & Experimental Ophthalmology, 50(4), 386–397. https://doi.org/10.1111/ceo.14050
- Hastings G, Applegate R, Nguyen L, Kauffman M, Hemmati R, Marsack J. No date. Comparison of Wavefront-guided and Best Conventional Scleral Lenses after Habituation in Eyes with Corneal Ectasia. Optom Vis Sci, 96(4), 238–247. https://doi.org/10.1097/OPX.0000000000001365
- Maeda N, Nakagawa T, Kosaki R, Koh S, Saika M, Fujikado T, Nishida K. (2014). Higher-Order Aberrations of Anterior and Posterior Corneal Surfaces in Patients With Keratectasia After LASIK. Investigative Opthalmology & Visual Science, 55(6), 3905. https://doi.org/10.1167/iovs.14-14391
- Gelles J, Su B, Kelly D, Brown N, Wong J, Yoon G, Pfeifer, T, Erdman C, Hersh P, Greenstein, S. (2024). Visual Improvement With Wavefront-Guided Scleral Lenses for Irregular Corneal Astigmatism. Eye Contact Lens. https://doi.org/10.1097/ICL.0000000000001152. Epub ahead of print.
Daniel Moriarty is an optometrist based in Adelaide with a clinical focus on optics, keratoconus and scleral contact lenses. He currently serves as the South Australian president of the Cornea & Contact Lens Society of Australia (CCLSA).