Trade winds & trendy terms at WGC
It’s amazing how many medical conferences are held in Hawaii – a clear testament to what an excellent environment it is for learning. There is a large convention centre beside the river, a stone’s throw from Waikiki beach, the air is warm and Hawaii gets the trade winds, which prevent it from getting too hot and make it as much a good place to sail and surf as it is to learn.
The 11th World Glaucoma Conference (WGC) in Honolulu was opened by a Hawaiian who explained the hidden depths of the local greeting, ‘Aloha’. ‘Alo’ refers to our faces and ‘ha’ conveys the meaning of breath. When you get close to someone’s face, your noses and foreheads touch and you share the air between you, which creates a bond conducive to learning and the candid exchange of views.
There were clear differences in tone between WCG2025 and WGC2023 in Rome. Certainly Rome was hotter and the conference more extravagant and it directed delegates to, “do more cataracts for glaucoma indications; do more MIGS”, and the trade display was significantly larger. However, Hawaii generated a feeling of participation and had a great subject range with considerable depth of clinical and surgical topics.

Prof Graham Lee, with Drs Mia Zhang, Paul Chew and Stephen Best
For the introduction, WGC founder Professor Bob Weinreb presented a geographical analysis of glaucoma literature from the turn of the 20th century until now, which showed the bulk of glaucoma research being produced by the US, but also highlighted the very rapid rise of the Chinese contribution since 2008 and also the considerable contribution of Australasia, which is remarkable for our comparatively small size.
There has been a steady 5% per annum growth in the number of glaucoma papers published. Social network analysis showed connections between centres of ophthalmology research, which were represented by pathways of various breadths and something which Prof Weinreb took as a sign of a very healthy and competitive research and innovation eco-system. According to the Harvard Gazette, the health research ecosystem is made up of universities, the life sciences industry and the National Institutes of Health and has been nurtured since its origins in World War II, when mass production of penicillin was a strategic imperative.
Glymphatics tissue network
Professor Neeru Gupta gave an update on research into the clearance of tissue fluid in the brain, optic nerve and eye. She asked, “Where does the waste from the body’s most metabolically active tissue (retina) go?” The brain does not have vascular lymphatic channels and the term ‘glymphatics’ has been coined to describe the network of glial tissue in the brain and retina which is responsible for clearance. Prof Gupta’s studies (with Dr Alexander Thrane in 2021) have shown that cerebrospinal fluid is not confined to the subarachnoid space but enters the optic nerve along astrocyte-lined routes and that retinal waste enters the optic nerve. The concept of glaucoma as a clearance disease is a very important new idea.

Front middle: Dr Mousindha Arjunan; left to right: Dr Mia Zhang, Dr Shenton Chew, Lucy Best, Henny Best, Dr Stephen Best, Deborah Chan, Dr Aaron Wong, Robyn Stirling and Dr Jesse Gale
Following on, Professor Ningli Wang of Beijing Tongren Eye Centre gave a plenary paper on the ‘dual pressure model’ of glaucoma, when the optic disc and lamina cribrosa are affected by the difference between the intracranial pressure (ICP) and intraocular pressure (IOP). Simply: if the IOP is high or the ICP low, there are conditions for cupping and glaucomatous optic neuropathy. Prof Wang focused on the perfusion of the lamina cribrosa in dual-pressure scenarios. Low intracranial pressure has been found in people with normal-tension glaucoma (NTG) and alternative treatments for this are required, especially as most patients with glaucoma in Asia have NTG. Prof Wang observed three modifiable factors in his NTG patients: a low BMI, low diastolic blood pressure and low vitamin A.
The happiest moment in the first plenary session was the announcement at its conclusion that the 2027 World Glaucoma Conference is to be held in Kyoto, Japan.
OCT in great detail
The role of OCT in glaucoma management was discussed in great detail at more than one session. ‘Temporalisation’ is the name for how the superior and inferior retinal nerve fibre bundles emerging from optic discs are displaced temporally in patients with myopia. This helps explain why, when patients with myopia are compared to proprietary databases, the analysis often mistakenly indicates thinning of the superior and inferior retinal nerve fibre layer (RNFL) – typically flagged in red on reports – a phenomenon known as 'red disease’. The key thing here is carrying out a careful thickness analysis, checking for symmetry and watching for progression.
Dr Ki HoPark (South Korea) focused attention on the macula OCT, showing that glaucoma can be detected very early in cases where there is thinning of the inferotemporal-macula, especially if this thinning is progressive. This type of thinning gives rise to the temporal raphe sign otherwise known as a 'snail sign’. Progressive macular thinning occurs before visual field changes. The 10° field is most sensitive to the macular and this glaucoma pattern is found most often in NTG.
Dr Sanjay Asrani (US) walked us through OCT glaucoma masqueraders; he gave so many examples of cases where they looked for all the world like glaucoma but in fact were not! For example, cotton wool spots (CWS) can occur for a variety of reasons and are found in a variety of sizes, sometimes as loners – but often not – and they come and go. Each CWS represents an infarct in the inner retina and will have permanent functional and structural consequences. The way to distinguish CWS from glaucoma, is if the RNFL thinning does not extend to the disc and there is inner retinal thinning with sometimes a small tractional notch in the outer retina. Another masquerader was a cancer-associated retinopathy which, of course, you wouldn’t want to miss.

Robert Ng, Erin Jourdain, Deborah Chan, Robyn Stirling, Dr Shenton Chew, Dr Aaron Wong, Fiona Suter, Dr Anthony Suter, Dr Mark Donaldson (author) Dr Dickson Wong, Dr Stephen Best, Dr Keith Maslon and Dr Mia Zhang
Meeting Prof Asrani was a highlight and he privately told me that he pays great attention to the total thickness of the retina when assessing macular OCT – there is less floor effect from thinning and less of a problem with instrument registration of multiple retinal layers.
In terms of other diagnostic help, we were told ROTA, or retinal nerve fibre layer optical texture analysis, is a method of imaging glaucomatous nerve fibre layer defects that uses unique combinations of OCT data. It is significantly more sensitive at detecting glaucoma defects than OCT alone or red-free photography. This technology is a patented Chinese innovation and bypasses reliance on normative databases. I would like this loaded onto my OCT ASAP, please.
There was also an update on the Ocular Hypertension Treatment Study (OHTS 1999), which said the data was linked to polygenic risk scoring, increasing the predictive power of the study significantly.
I was very keen to find out how the Glaucoma Nicotinamide Trial is going and can report that recruitment for the international multicentre trial is at 50%. A new nutrient – pyruvate – has been added to the mix and attested to in rodent models and, apparently is easily procurable as part of a body-building product, as humans who like treadmills will know.
In addition to the nicotinamide trial, in which all subjects are treated for glaucoma, the Swedish arm of it has started enrolling untreated early glaucoma patients, who will be randomised to nicotinamide or no treatment at all.
Glaucoma surgery pearls
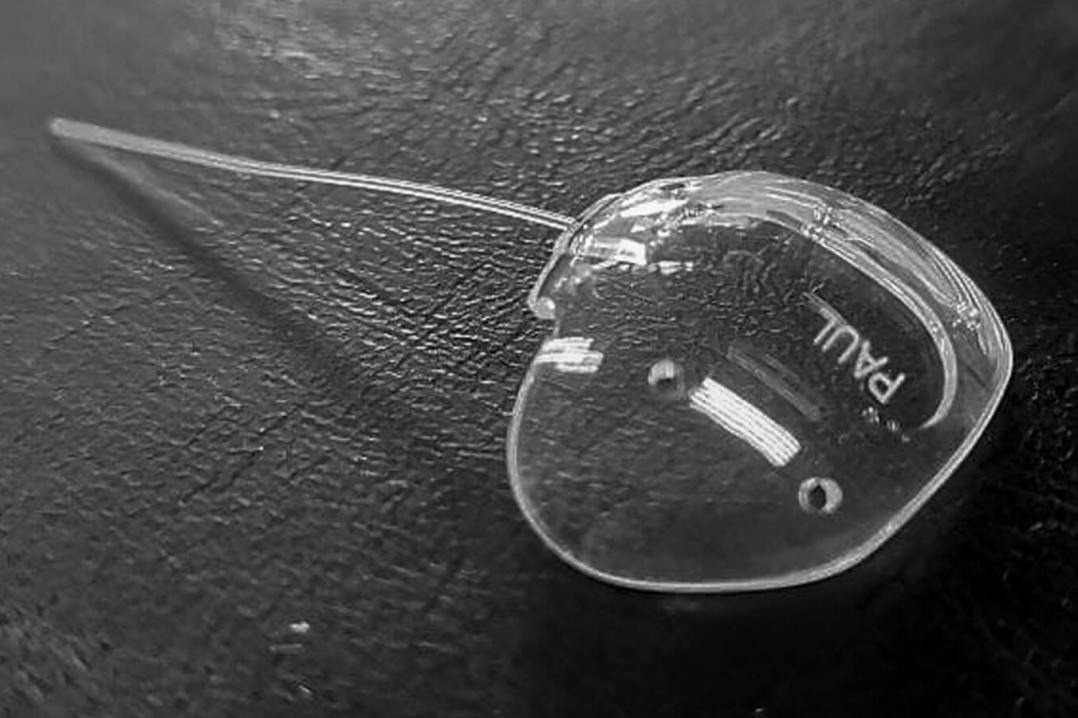
It was great to see glaucoma surgery was comprehensively discussed, with lots of surgeons candidly discussing techniques, caveats and complications and lots of surgical video. The tube and plates were discussed and a special breakfast session with Dr Paul Chew, inventor of the Paul Tube, was well attended. The Xen and Preserflo were also discussed as were the Hydrus and Glaukos iStent. Interactions of glaucoma surgery and cataract and management of complications were also thoroughly scrutinised.
The congress’s film festival winner was a beautiful presentation of function-preserving techniques of bleb rescue surgery from India. And New Zealand’s Dr Shenton Chew also gave an excellent talk on managing late failing blebs.
Dr Ike Ahmed, who coined the term ‘minimally invasive glaucoma surgery’ (MIGS), presented several papers at the Abbvie Xen Symposium. MIGS is definitely a successful marketing term as it sounds so cool that everyone wants to say they do MIGS and have MIGS done to them and a lot of operations come under the heading of MIGS. So let me introduce you to MIBS – I learnt in Honolulu that MIBS stands for minimally invasive bleb surgery. Being aware of the marketing popularity of the term MIGS, I suspect someone is having a laugh. The MIBS sessions included all the operations that produce blebs and revise blebs. I would be surprised if MIBS survives to the next conference.
Angle closure featured prominently across multiple sessions, culminating in a meeting of the consensus committee, which plans to publish updated guidance on angle closure later this year. The committee functions as a sort of nomenclature watchdog and there have been a few changes to the terms we were getting used to. It has proscribed the use of the term ‘malignant glaucoma’, hereafter to be referred to as ‘aqueous misdirection’, despite all of us understanding what malignant glaucoma meant. The reason given was that it is a historic term (like glaucoma is a historic term).
PAC, BANG and SPAC
The committee has also introduced two new categories: primary angle closure disease (PACD), consisting of primary angle closure (PAC) and primary angle-closure glaucoma (PACG) and spectrum of primary angle closure (SPAC). Personally, I think that glaucoma was always the perfect word for the spectrum of glaucoma and wish the word hadn’t have been appropriated to mean only glaucomatous optic neuropathy. The full list of changes will be published by Kruger later this year. In the meantime, the English language will cope.
Angle surgery was discussed, with Glaukos iStent a very big player in the goniotomy space. It’s a high-profile US company with deep pockets like Alcon, which has the Hydrus, but in many countries there is simply not the money for implants. Reflecting this, there were many non-implant goniotomy techniques presented. New players in the goniotomy space were the Tanito micro-hook technique and the bent ab-interno needle goniotomy (BANG).
A very able and charismatic surgeon, Professor Xiulan Zhang from Zhongshan Ophthalmic Centre, China, presented numerous videos of goniotomy in multiple scenarios including angle closure, which is generally not encouraged in our hemisphere. She demonstrated how to perform goniosynechialysis and, despite difficulties with pronunciation, she bravely held the floor and took many questions. It is great to see so many different approaches to glaucoma surgery.
It is important to include that the suprachoroidal space is still under investigation as a location for surgical intervention in glaucoma. The Cypass caused loss of corneal endothelial cells and is now history, however, the iStar Miniject – a spongy device – is available for implantation in Australia. Surgeons I spoke to are pleased and said that, as with all these innovations, there is a learning curve.
In the alternative space, no one at the WGC was supporting marijuana; however, we found meditation lowers IOP but requires a one- to two-hour daily commitment.
This was a truly great conference, with lots of Australians and New Zealanders attending and presenting; the venue was excellent and the networking opportunities fantastic. I suspect all attendees are looking forward to Kyoto in 2027.
Dr Mark Donaldson is a consultant ophthalmologist at Eye Doctors, Ascot Hospital and Greenlane Clinical Centre in Auckland, specialising in cataract and glaucoma surgery and medical retina. He is an honorary senior lecturer at the University of Auckland and a trustee of Glaucoma New Zealand.