Vabysmo funding potential causes submission flurry
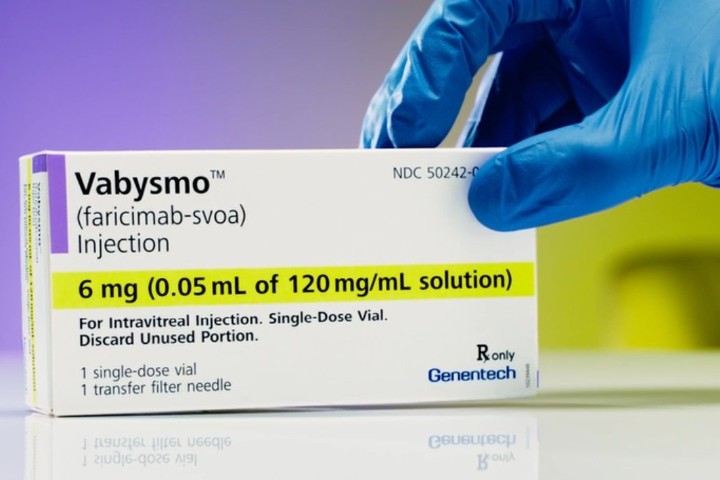
A Pharmac proposal to fund four new medicines from Roche, including the anti-VEGF treatment Vabysmo (faricimab) for neovascular (wet) age-related macular degeneration (nAMD) and diabetic macular oedema (DMO), resulted in several hastily despatched submissions from the eyecare industry.
The proposal, released on 24 September with a submission deadline of 8 October, was welcomed by Roche. However, senior ophthalmologists and eyecare groups were disappointed Pharmac only proposed funding Vabysmo in public hospitals (described in Health New Zealand jargon as ‘PCT-only’) and only as a second-line treatment for patients who hadn’t responded well to the standard Avastin (bevacizumab) injections.
“The proposal for PCT-only will negatively impact patients and the New Zealand healthcare system,” said Macular Degeneration New Zealand (MDNZ) in its submission. This will lead to poorer visual outcomes for patients due to delayed treatments, increased waiting times and time away from paid employment, plus increased costs to the health system, wrote MDNZ general manager Sarah Berman.
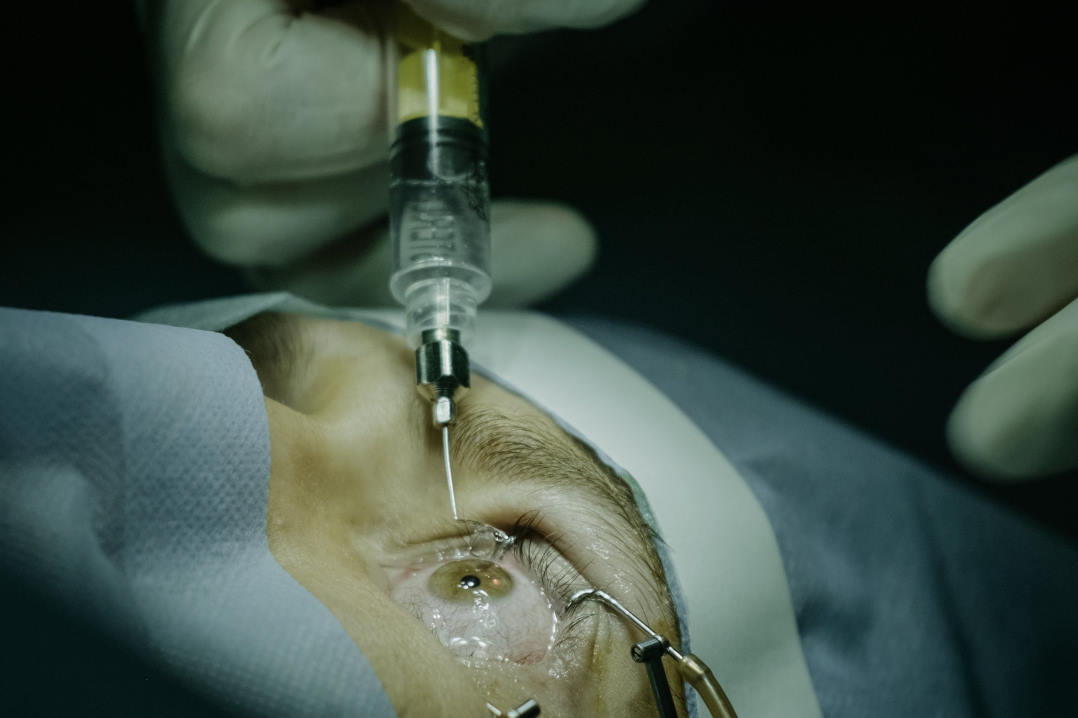
Given faricimab’s proven efficacy compared with other anti-VEGF treatments (as shown in the Avonelle-X, Faretina, Farwide and Truckee studies) and reduced injection frequency, allowing patients to move from monthly to three-monthly injections, it can improve visual outcomes and the quality of life for patients, especially for those with treatment-resistant eye disease, said Tauranga Eye Specialists’ Dr Andrew Thompson. This reduces the burden on patients and results in cost savings as there are fewer clinic appointments and injections required, he said. “The current Pharmac proposal to fund only public patients is concerning and will result in a transfer of cost from private to public care and the overloading of public eye health services.”
In an open letter to David Seymour, associate minister of health (Pharmac), the chair of RANZCO NZ, Dr Liz Insull, explained that, unlike cancer medications, there’s no insurance funding for anti-VEGF injections. “Clearly most patients will want to access the better drug and will therefore demand to have their treatment given in a public hospital if the alternative … would mean they would have to pay for the medication themselves, increasing the burden on the public hospital system.” Such a model also seems contrary to Pharmac’s mandate in the Pae Ora (Healthy Futures) Act, she wrote, which is, “To secure for eligible people in need of pharmaceuticals, the best health outcomes that are reasonably achievable from pharmaceutical treatment and from within the amount of funding provided.”
Public eye clinics are already drowning under the weight of injections and will become even more swamped if patients transfer from the private sector, said Christchurch specialist Dr Ainsley Morris. “Waiting times for injections will increase, vision will be lost, more money will need to be allocated to meet demand. And then there are all the other patients with other ophthalmic conditions who won’t be able to access care and treatment because funding is allocated to AMD patients.”
In a joint submission, Retina Specialists’ Dr Leo Sheck, on behalf of the Ophthalmology Surgical Group in Health NZ Auckland (Central), Christchurch-based Dr Oliver Comyn, on behalf of the NZ Save Sight Society, and Dr Thompson said there were 14,395 anti-VEGF injections in Auckland in 2019 and this had increased to 17,102 in 2024. “Adding excess patients to this already very stretched system by making faricimab PCT-only will crack our public ophthalmology system and make all our injection patients worse off due to delay of care.”
Drs Comyn, Thompson and Sheck also noted that public ophthalmology services in Tauranga and Rotorua are provided by private clinics under a joint-venture model. Thus, if faricimab was PCT-only, public patients in both these regions would be unable to access it, they said.
It's also unfair that Pharmac is only proposing to fund faricimab as a second-line treatment for patients who haven’t responded well to Avastin, said submitters, not patients who’ve failed to respond to Eylea (aflibercept) or Lucentis (ranibizumab). “Around 10% of AMD patients treated with aflibercept do not fully respond to treatment, with ongoing fluid and inability to extend treatment intervals beyond four weeks,” wrote Berman. “The clinical risk of this group of patients is exactly the same as those who have persistent fluid despite bevacizumab treatment, who will be funded for faricimab. If eligibility criteria for the Special Authority were added to enable treatment for patients who have failure on a second-line agent, then this group of patients will not be discriminated against.”
Pharmac’s decisions are guided by robust clinical evidence, advice from health professionals, and the lived experiences of people affected by various health conditions, said Pharmac’s acting manager of pharmaceutical funding Claire Pouwels. “As part of our assessment, we’ve considered how this proposal would benefit people and how it compares to other medicines we could fund. This proposal also reflects the scope of the funding application we received for faricimab. We have not received a funding application for other groups or lines of treatment, but we would welcome one.”
Roche’s funding application for Vabysmo sought access for the treatment of nAMD and DMO in patients whose disease remains uncontrolled despite three intravitreal doses of off-label bevacizumab, said Dr Kerryn Symons, Roche NZ’s country medical director. “We proposed similar access criteria to aflibercept, which currently allows funding in both public hospitals and community/private settings. We will continue working with Pharmac to achieve broad access to faricimab for all patients who could benefit from this treatment.”
Pouwels stressed that no decision has been made yet. “We’ve received valuable feedback about how this proposal could impact services and patient outcomes, which will be taken into consideration when making a decision.” The proposal and the feedback will be assessed by Pharmac’s board in November, she said, with a decision made soon after and, if approved, funding would be available for faricimab from 1 December this year.