When in Rome… for the World Glaucoma Congress
The 10th World Glaucoma Congress (WGC) in Rome was the largest yet, with 3,000 attendees and 1,000 abstracts accepted. The Eternal City was hot, sunny and heaving with tourists as we arrived at La Nuvola (The Cloud), the award-winning, 30m-high, glass-and-steel masterpiece hosting this year’s WGC. Its huge, organically shaped auditorium is seemingly suspended from the ceiling of the structure with entry via three long parallel escalators. The welcoming ceremony saw the faculty individually introduced onto the stage, with lights flashing in time to DNCE’s ‘Cake by the Ocean’ (thank you Richard Johnson for identifying the score). The welcome concluded with a beautiful, if incongruous, operatic rendition of ‘Time to Say Goodbye’.
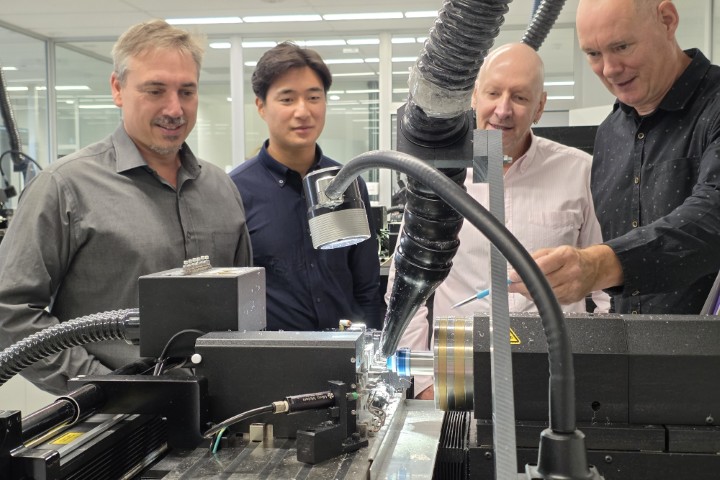
Distinguished Professor Robert ‘Bob’ Weinreb, from the Shiley Eye Institute at the University of California San Diego, was the recipient of the Congress Laureate award and set the conference agenda with his acceptance speech. As the co-founder of the World Glaucoma Association, Prof Weinreb was quick to recognise the value in uniting disparate glaucoma societies around the globe. He also holds chairs in ophthalmology and bioengineering and data science, is a prolific investigator and can name 64 professors from among his fellows. He enthused about big data, specifically smartphones as diagnostic tools. These can easily photograph an optic disc, store and access personal medical information and assist with therapy, he said. He was also keen on the potential for intraocular pressure (IOP) sensors that interface with smartphones and the internet. “What we need is an implantable pressure-measuring device,” he said.

Distinguished Professor Robert ‘Bob’ Weinreb
Artificial intelligence (AI) is also a player in Dr Weinreb’s future vision of glaucoma care. Partly acknowledging concerns around AI, without describing their breadth, he asked if we were ready for a doctorless world where the patient carries their own information from provider to provider? He reassured us, however, that AI will usher in far better decision-support and thus actually enhance our role as doctors.
With internet-based resources becoming increasingly sophisticated, the roles of benefactor and beneficiary are unclear, however. I don’t see that an implantable sensor is of benefit to patients; it seems more like a benefit for scientists and surgeons and a risk for patients, unless it were linked directly to a very effective treatment. Does an AI world where large amounts of data are owned and carried by patients and where ‘nudgings’ are operative, constitute autonomy for all patients?
Genetic influences and passions
Patients with an inheritance pattern of glaucoma are a minority but are relatively easy to pick out from their family history. For most glaucoma cases we see, a range of genetic factors are at work. If all the genes known to have a glaucoma effect are screened for, then a polygenic risk score, based on the sum of the genes weighted for the significance of each, can be assigned.
This polygenic risk can be scored and was promoted at the industry display. But how useful will it really be? The experts asserted ophthalmologists won’t wait for the results before deciding on a management plan. That seemed sensible, because we already work this type of risk into our assessments when we enquire about family history of glaucoma and gauge its severity in family members.
The president’s address was given by Professor Roy Wilson, president of Wayne State University, who encouraged us to review how we factored race into our patient assessments. He provided an example of three leaders in genomics research who demonstrated more genetic similarity between two people of different races than two of the same race. Then he invited us to prefer genetic assessments to racial assessments in all our practices, saying there’s a greater need for precise disease disparity biomarkers than for race. However, he acknowledged race remains a handy shortcut for many situations, especially where rates of intermarriage are low. He also made the point that social and economic conditions are primarily accountable for ethnic health disparities, rather than genetics.

Prof Roy Wilson discusses race and glaucoma
The WGC 2023 presenters’ enthusiasm for genetic testing was unbounded. In the future, eye health professionals will source everyone’s genomic information, gleaned at birth, from a central repository. In theory, this will allow medical interventions at a much earlier stage than happens now. However, it’s not clear if such a repository will be held by a health authority, an insurance provider or the government. But for me, it’s a polite no, thank you! I am not carried by their enthusiasm. The most enthusiastic supporters of a population-based genomic approach seem to be public health doctors and epidemiologists, who view patients collectively. Their concepts of good or bad outcomes are from their own assumptions and are disconnected from the wishes, realities and the privacy requirements of individuals.
Moorfields’ Dr Anthony Khawaja’s presentation on his research showed a very tight association between genetic risk of glaucoma and IOP elevation. In his opinion, the number of patients labelled as ‘normal-tension glaucoma’ are very much inflated, which nicely aligns with investigations on IOP measurement. We measure IOP infrequently, and studies using animal models and the latest iteration of Sensimed’s Triggerfish contact lens show what was always suspected: IOP varies constantly. The Triggerfish has actual manometry but at the expense of acuity, since the pressure sensor is in the visual axis. Within a glaucoma practice, most patients under observation are stable on one or two medicines. About 5% of the practice population are fast progressors, who are the important people to identify. They may be new patients, but some will be stable patients moving into an accelerated phase.
The WGC’s 2023 faculty of glaucoma influencers reminded us of Moorfields’ Professor Sir Peng Khaw’s 10-10-10 glaucoma surgery wish. He said what glaucoma needs is an operation that takes 10 minutes, will last for 10 years and will provide a reliable IOP of 10mmHg.
MIGS messages to neuroprotection
Minimally invasive glaucoma surgery (MIGS) was discussed at length. There was a strong message from presenters that surgical intervention in glaucoma should include earlier lens surgery, which also provides an opportunity for an angle intervention (or two). The stated aim is to reduce the medication burden on patients and increase compliance. Surgery options available globally for transcanilicular surgery include Helios, an excimer laser which makes perfect circular perforations in the trabecular meshwork through to Schlemm’s canal; Glaukos’ iStent; Alcon’s Hydrus; and, for the cost sensitive, there is the old but effective trabeculotomy, often undertaken with a Prolene suture and called gonioscopy-assisted transluminal trabeculotomy (GATT). For ab interno full-thickness angle stenting there is Xen (AbbVie), which comes in the newly available 63µm lumen, as well as the standard 45µm lumen. For ab externo use there is Preserflo (Glaukos). To improve the flow in the distal collector network there are options for gently forcing viscoelastic into Schlemm’s canal, including the iTrack (Nova), manufactured at the Molteno factory in Dunedin. These methods decrease IOP by increasing outflow facility and leave no stent behind. There is endoscopic laser cyclophotocoagulation, whereby laser can be directly applied to the ciliary body at the time of cataract surgery, thereby reducing IOP by reducing aqueous inflow.
The partial thickness transcanalicular procedures are often compared to selective trabeculoplasty (SLT) in terms of efficacy. Leaving angle surgery, direct-SLT is a new way to laser directly (the laser passes through the sclera to the target tissue) using sophisticated eye-tracking. This is being promoted by Belkin Vision and has the advantage of requiring no gonioscopy and is easy to apply. This is definitely a mass treatment tool that could be of great interest in New Zealand.
With neuroprotection research advancing, the Centre for Eye Research Australia’s Professor Jonathan Crowston brought us up to date with his nicotinamide (vitamin B3) trials, but said the link is not yet proven and cannot be recommended. Studies presented by Duke NUS’ Dr Vicky Chrysostomou threw light on the mechanism of action of moderate exercise in improving health. Mice subjected to optic nerve crush injury and randomised to moderate exercise recovered more function compared to controls, which she linked to increased levels of brain-derived neurotropic factor. The health benefit was lost if the poor things were exercised too strenuously, however.
The conference ended with a gorgeous casual dinner in the heat of Rome and more joyous operatic singing. This was a conference to remember and purged the funk of lockdown. Hopefully we can look up and forward to continued normality.

Dr Mark Donaldson is a consultant ophthalmologist at Eye Doctors, Ascot Hospital, and Greenlane Clinical Centre in Auckland, specialising in cataract and glaucoma surgery and medical retina. He is an honorary senior lecturer at the University of Auckland and a trustee of Glaucoma New Zealand.