Optic disc pit with maculopathy
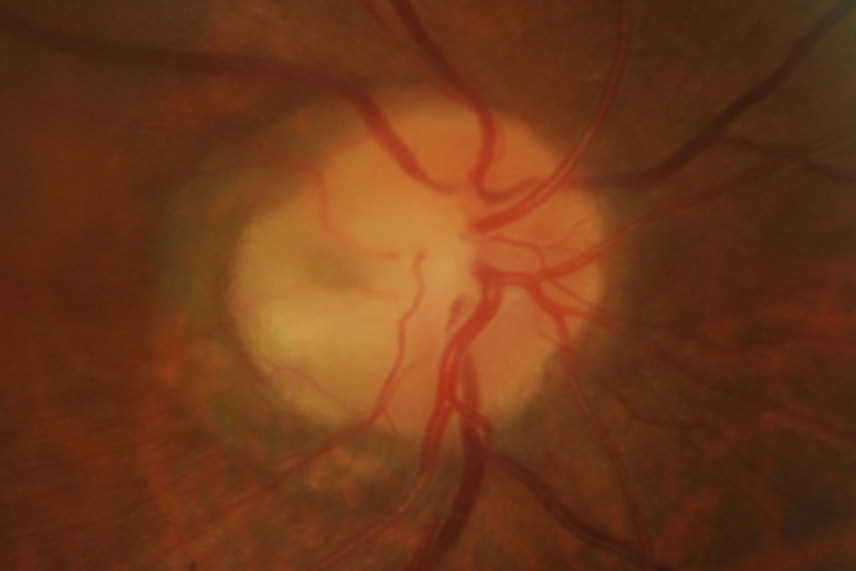
A 58-year-old male with no underlying medical history was referred for retinal oedema adjacent to the optic nerve head with cystic changes and a shiny appearance on the overlying retina for the right eye. Unaided visual acuity was 6/9 and 6/6. He was asymptomatic and was incidentally noted to have macula oedema during a routine examination. The anterior segment examination was normal, but the right eye optic disc assessment showed a greyish-white depressed area in the temporal quadrant (Figs 1 and 2) along with cystic changes at the macula. The left eye examination was normal. OCT examination of the right eye showed schisis-like separation of retinal layers, most marked in the outer retinal layers, extending up to the optic disc temporal margins (Fig 3). There appeared to be a clear communication between the optic disc and the schisis-like separation of outer retinal layers.
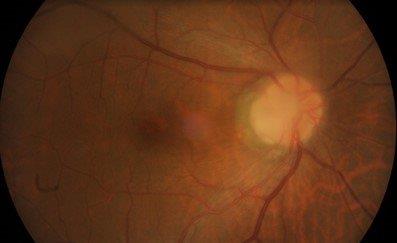
Fig 2. Fundus photograph of patient’s right optic disc pit with subtle-appearing maculopathy with a small amount of
reduced definition of the background choroidal vessels near the papillomacular area
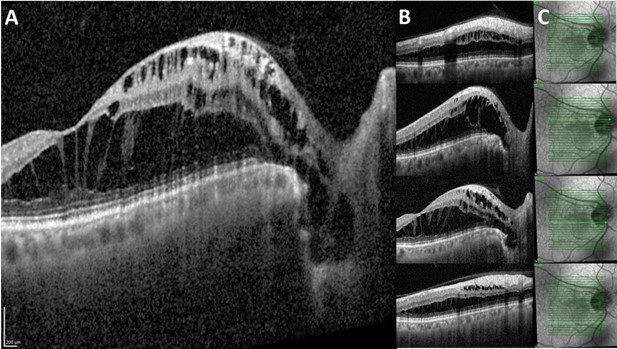
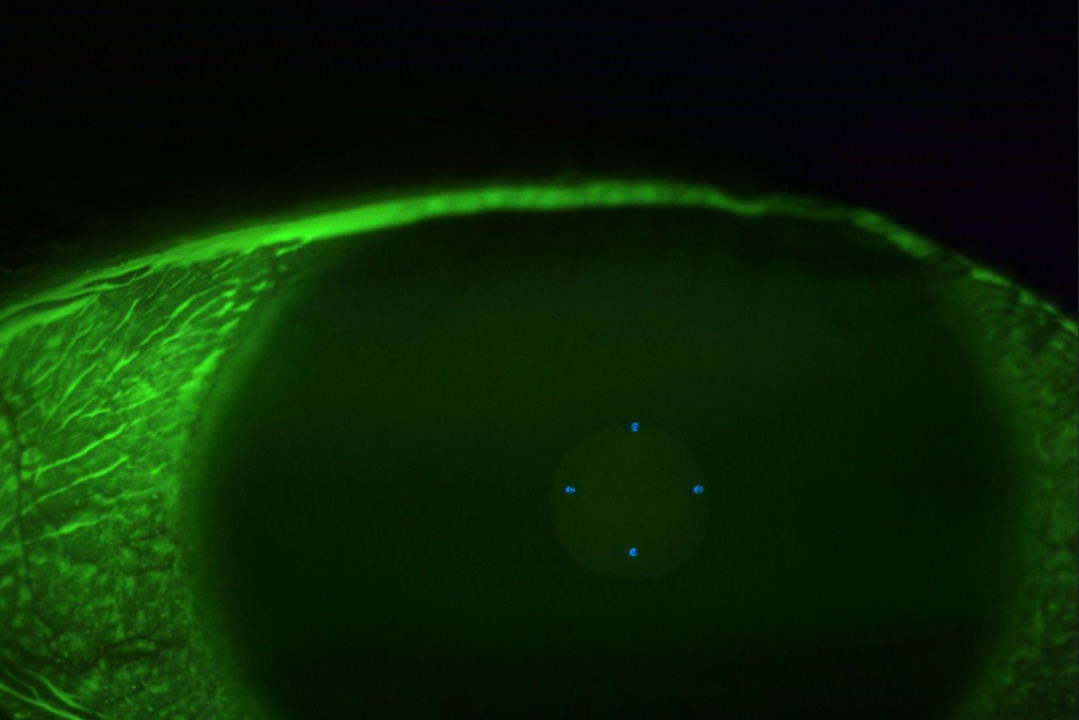
Fig 3. OCT at different sections of patient’s optic disc pit maculopathy. A) The fovea and the disc displaying the
hyporeflective space extending from the base of the optic nerve head and throughout the retina, causing separation of
multiple retinal layers. C) En face infrared reflectance with light-green arrow corresponding with the marker in B
A diagnosis of right eye optic disc pit (ODP) with maculopathy was made. As the patient was asymptomatic and did not want surgical intervention, it was decided to follow up conservatively.
Discussion
ODPs are rare congenital defects of the optic disc, commonly located on the inferotemporal side1, although they could be located in any optic nerve quadrant. ODPs are thought to arise from the incomplete closure of the optic fissure and form a part of the spectrum of congenital optic disc anomalies which includes optic disc colobomas, morning glory anomalies and extrapapillary cavitation2. The reported prevalence varies from 1 in 4,000 to 1 in 11,000 of population 3,4. Although it is commonly unilateral, it is bilateral in 15% of patients5. There is no gender predisposition6.
Clinically, ODP usually appears as a greyish-whitish, round or oval depression of the optic disc (Fig 1), and it may have different levels of severity. More than half of the patients in their third or fourth decade go on to develop maculopathy. Typically, OCT demonstrates fluid in the sub-retinal and intra-retinal compartments. The outer retinal layers are more commonly affected and the OCT demonstrates schisis-like separation of the outer retinal layers. Very often, schisis-like separation of the retinal layers extends to the optic disc pit, as seen in this case.
An ODP may be in any quadrant of the optic disc pit. It is rare for non-temporal ODPs to cause maculopathy. These patients are often asymptomatic but may have visual field defect due to the defect in the optic disc, which is often detected during routine examination. Non-temporal ODPs have the potential to be misdiagnosed as normal-tension glaucoma (NTG). The superior or inferior ODP may be misdiagnosed as optic-disc suspect and, in the presence of an associated visual field defect, can be potentially be misdiagnosed as NTG.
The origin of the fluid responsible for maculopathy is not yet completely understood, but several have been proposed:
- Vitreous fluid: maculopathy is commonly seen in the third or fourth decade of life, with vitreous syneresis commonly seen in this age group
- Cerebrospinal fluid: often the schisis-like separation is seen extending up to the depression of the ODP and there appears to be a clear communication between these two spaces. Silicone oil has been found in the cerebrospinal fluid on lumbar puncture following retinal surgery with silicone oil tamponade. This suggests a possible communication between the intraocular (ODP and intra-retinal space) and subarachnoid compartments (with cerebrospinal fluid)
- Leaking retinal vessels
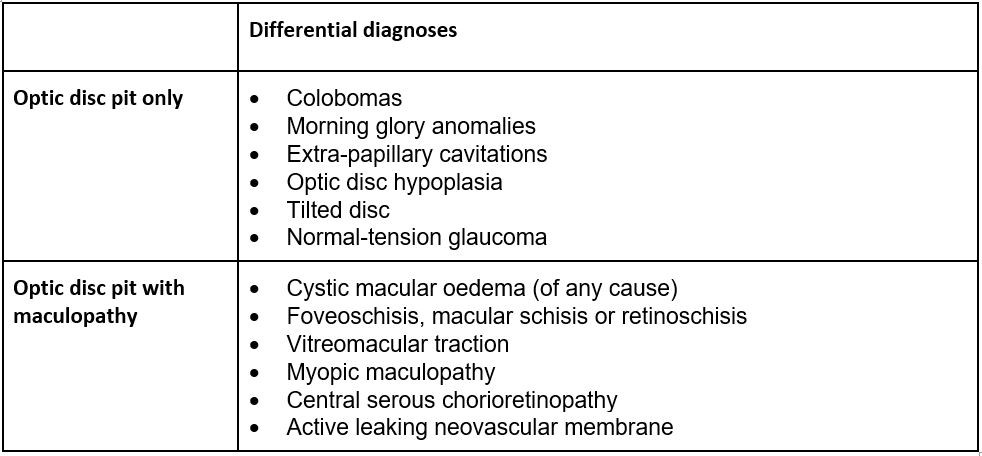
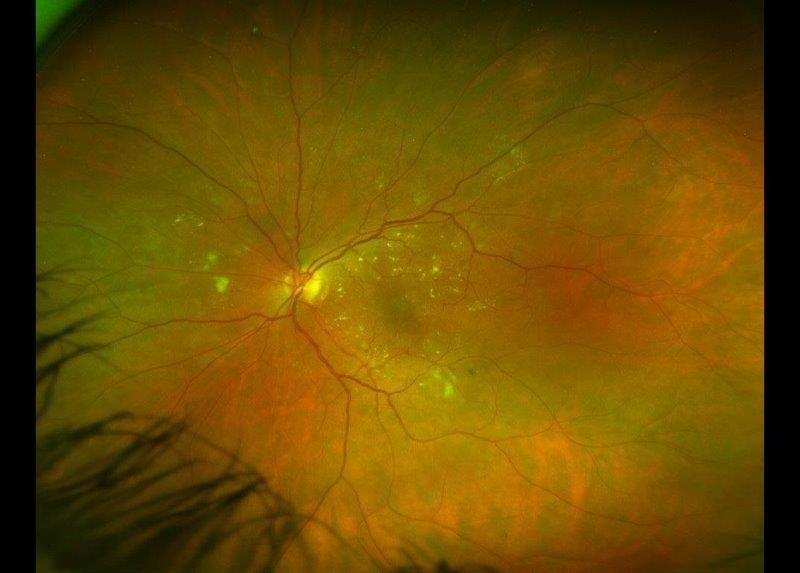
Table 1. Differential diagnoses: signs of optic disc pit overlap with several more common diseases
Prognosis
ODP maculopathy is seen in up to half of the patients with ODP in the temporal quadrant of the optic disc. The maculopathy resolves spontaneously in about a quarter of these patients, with variable impact on vision in the remainder. Vision tends to remain normal in patients without maculopathy6-8. Patients with ODP in other quadrants can have non-progressive visual field defect, which is usually detected during routine examination1,9.
Management
ODP without maculopathy can be monitored. Due to the potential progression of maculopathy in the third- and fourth-decade age group, these higher risk patients should be followed up closely with regular OCT. In the presence of maculopathy affecting vision, different treatment options can be considered, the most successful being pars plana vitrectomy with inner limiting membrane peel, endolaser and tamponade.
Key points
- ODPs, with or without maculopathy, are rare; however, they can mimic more common retinal conditions
- ODPs can be monitored routinely if there is no maculopathy or if vision is unaffected
- Patients in their third and fourth decade with optic disc pits can progress to maculopathy
- Maculopathy in optic disc pits can affect vision to a variable extent
- Non-temporal ODPs can be potentially misdiagnosed as normal-tension glaucoma
References
- Moisseiev E, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: when and how to treat? A review of the pathogenesis and treatment options. International journal of retina and vitreous. 2015;1(1):1-9.
- Jain N, Johnson M. Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. American journal of ophthalmology. 2014;158(3):423-35.
- Wang Y, Xu L, Jonas J. Prevalence of congenital optic disc pits in adult Chinese: The Beijing Eye Study. SAGE Publications Sage UK: London, England; 2006.
- Gordon R, Chatfield R. Pits in the optic disc associated with macular degeneration. The British Journal of Ophthalmology. 1969;53(7):481.
- Brodsky M. Congenital optic disk anomalies. Survey of ophthalmology. 1994;39(2):89-112.
- Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefe's Archive for Clinical and Experimental Ophthalmology. 2011;249(8):1113-22.
- Yuen C, Kaye S. Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: a case report. J aapos. 2002;6(5):330-1.
- Gupta R, Choudhry N. Spontaneous resolution of optic disc pit maculopathy after posterior vitreous detachment. Canadian Journal of Ophthalmology. 2016;51(1):e24-e7.
- Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Archives of ophthalmology. 1988;106(1):61-7.

Dr Arvind Gupta is a consultant ophthalmologist specialising in cataract, medical retina and neuro-ophthalmology. He is based at Manukau Super Clinic, Greenlane Clinical Centre and Eye Doctors in Auckland.

Kenny Wu is a therapeutic optometrist at Eye Institute and Te Whatu Ora Counties Manukau. He has a clinical background in ocular surface disease and medical retina.