ANZCS 2018
This year's annual Australia and New Zealand Cornea Society (ANZCS) meeting was held in Sydney in February and was organised by Drs Con Petsoglou, Noni Lewis and Chameen Samarawickrama and Jane Treloggen from the NSW Tissue Bank.
The well attended meeting, originally developed by Professor Douglas Coster in the 1980s, is now in its 35th year. The venue for this year’s gathering was the InterContinental Hotel, set back from the bustling Circular Quay which had been wonderfully decorated for the 'Year of the Dog' Chinese New Year Festival.
In the first session, entitled ’Cutting Edge’, invited guest speaker Associate Professor Jod Metha of the Singapore National Eye Centre kicked off proceedings with an interesting talk on developing non-surgical therapies for TGFBI (transforming growth factor beta-induced gene) dystrophies by identifying peptide targets to reduce corneal opacity formation. Dr Greg Moloney then described his experiences introducing a successful keratoprosthesis service in Sydney, using the osteo-odonto keratoprosthesis (OOKP) technique, with his colleague and friend Dr Shannon Webber who provides maxillofacial expertise.
Professor Gerard Sutton from the Save Sight Institute introduced the iFix pen and iFix bio-ink, which was the winner of the inaugural ‘Big Idea’ research funding challenge last year. His 3D-printed technology promises the exciting prospect of a biocompatible transparent 'ink' delivered by a handheld device that actually facilitates cell proliferation and thus ulcer repair.
Dr Petsoglou and microbiologist Professor Wieland Meyer provided a detailed account of the recent 'therapeutic goods recall' by the Lions NSW Eye Bank following an apparent cluster of cases of candida endophthalmitis in DSAEK cases with pre-cut tissue. The honest and detailed account of the course of events and thorough investigation provided reassurance to surgeons of the quality and safety of service strived for.
The annual report from the Australian Corneal Graft Registry was received with interest, as usual. The number of DMEK cases continues to rise with good visual outcomes, but reduced survival compared with penetrating keratoplasty and Descemet’s stripping endothelial keratoplasty (DSEK) in-keeping with results from around the world. But the numbers remain small and the follow-up short for now. Professor Stephanie Watson presented the Keratitis Antimicrobial Resistance Surveillance Program (KARSP) update. Resistance remains low and is stable; others were encouraged to join the programme.
The first day concluded with a debate on whether femtosecond-assisted pterygium surgery was a 'welcome application of new knowledge’ (W.A.N.K.) or not. The fiercely argued cases for and against reflected the scientific but still humorous tone of the meeting! For now, at least, the audience was not swayed towards the femtosecond technique.
The relaxed and informal meeting dinner, hosted in The Pavilion in the Royal Botanical Gardens, was a welcome opportunity to catch up with colleagues and meet new friends, and was very well attended. It was a particularly pleasure to chat to invited guest speaker Dr Mike Straiko, from the Devers Eye Institute in Portland, Oregan, prior to his informative and instructive talk which began the DMEK session on Saturday morning. His presentation was full of videos and pearls of wisdom for those starting out with this often tricky to master technique for replacing Descemet’s membrane and the corneal endothelium with a true anatomical likeness. The significantly lower rejection risk of DMEK versus DSEK and PK and the improved quality of vision remains the significant attraction for mastering this technique. There were more tips to come the following day too, for those attending the Sydney DMEK course, organised by Dr Moloney, where Dr Straiko was joined by A/Prof Mehta and Drs John Males and Andrew Apel.
Later on the Saturday, Professor Minas Coroneo presented cases of ocular surface squamous neoplasia (OSSN) treated medically with retinoic acid and interferon, and topical cidofovir for refractory cases, with very promising success.
This year's Blandford Lecture was given by Professor Gordon Wallace of the University of Wollongong who provided a fascinating look at 3D bio-printing and its exciting potential applications in medicine and ophthalmology.
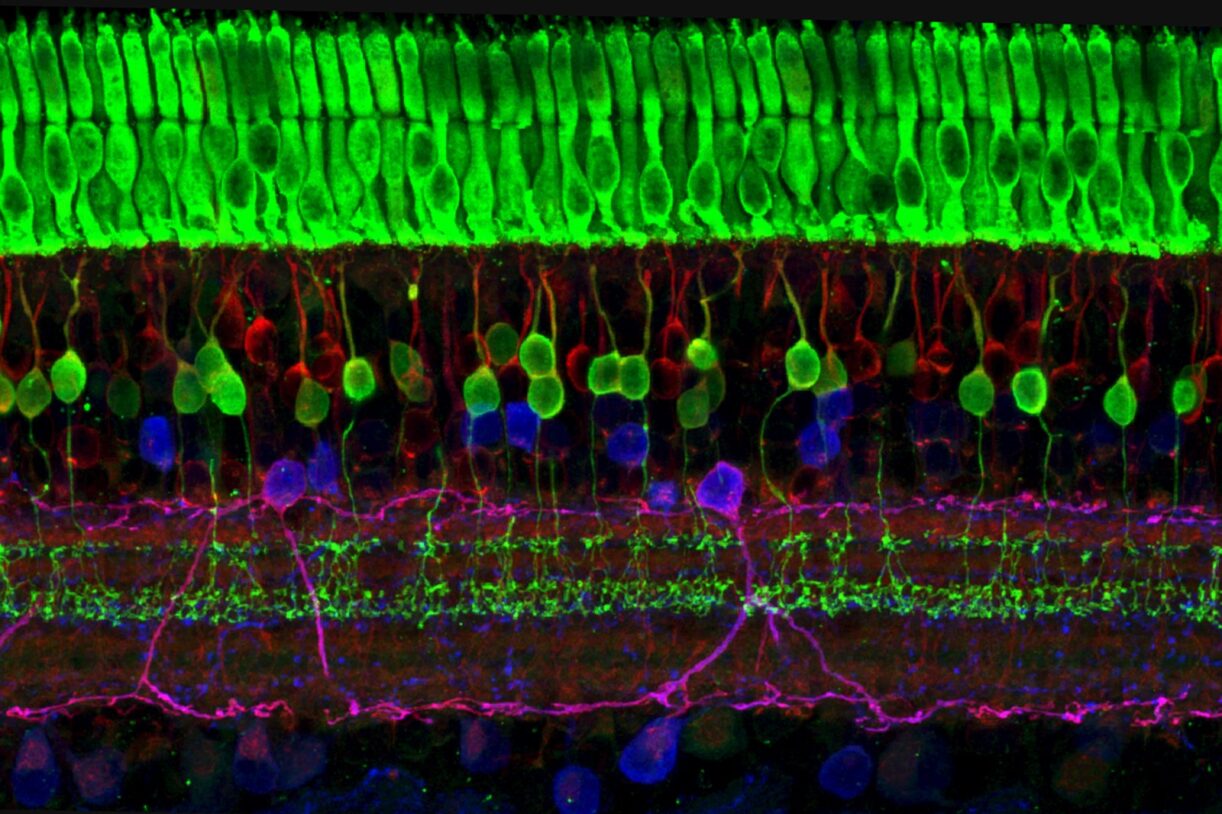
The next session focused on cross-linking with talks covering the use of a soft contact lens to allow treatment of thin corneas; iontophoresis; combining the treatment with intra-stromal corneal ring segments in anisometropic patients from asymmetric disease with clear corneas; and the effective treatment of children. Attention was drawn to the potential for rapid progression in children with need for close monitoring. The Doug Coster lecture titled 'Corneal endothelial cell engineering – it's not just culture' was given by A/Prof Mehta.
The afternoon then split into concurrent sessions on eye banking and ‘News from the lab’ focusing on dry eye, which included Auckland’s own Associate Professor Jennifer Craig as one of the speakers. Topics discussed in this session included how a poor blink can lead to ‘drop-out’ and atrophy of the meibomian glands and how blink exercises can be helpful; how intense pulsed light (IPL) can restore meibomian gland function with an accumulative effect; and how the cholesterol-lowering agent, atorvastatin, is being investigated as a novel treatment for evaporative dry eye.
Dr Tom Cuneen then shared how patients with Stevens Johnson Syndrome, the rare blistering skin reaction that can devastate the ocular surface, can benefit from early amniotic membrane transplant. He described his effective surgical technique that can be performed outside the operating theatre, if necessary.
The conference then ended with an interesting interactive complex case presentation and video session.
Overall the meeting provided open, in-depth discussion with informative and entertaining speakers in a friendly and informal manner. There is a lot of exciting research in the field of cornea and I, for one, am looking forward to seeing where bio-printing, corneal endothelial regeneration and novel treatments for previous 'surgical' diseases will take us next.
Dr Jennifer Court is a senior corneal fellow at the Department of Ophthalmology at the University of Auckland.