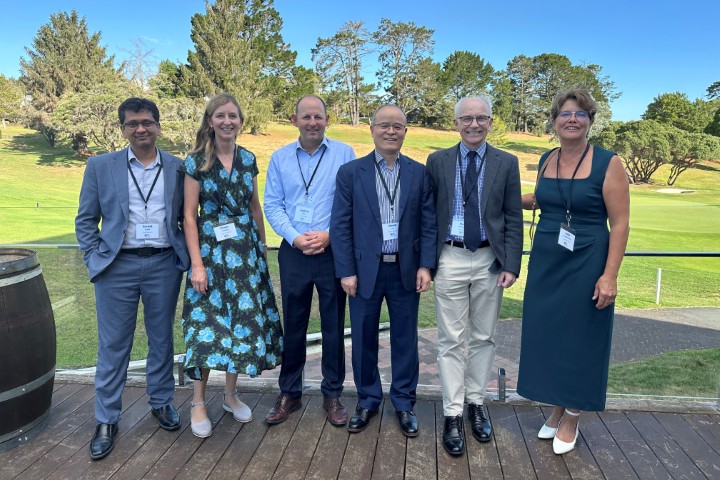
Eye Doctors celebrates 20 years
A record number of guests joined Eye Doctors’ alumni at the Remuera Golf Club to celebrate two decades of teamwork, community engagement and outreach work, and discuss several challenging cases at Eye Doctors’ first Grand Round for 2025.
Despite ex-Tropical Cyclone Alfred building in Brisbane, the evening’s keynote speaker and Eye Doctors co-founder Professor Shuan Dai had crossed the ditch from the Queensland Children's Hospital and Queensland University to be part of the celebrations. He kicked off proceedings with two unusual cases – one concerning multiple sclerosis and the other central nervous system glioma. Both were wrongly perceived to be vertical strabismus caused by fourth-nerve palsy, also known as superior oblique (SO) palsy. Prof Dai noted, however, that when there’s head tilt and torsion mismatch it can indicate an underlying and potentially life-threatening condition involving the cerebellum and/or brainstem. Think ocular tilt reaction (OTR) – a triad of skew deviation, head tilt and paradoxical conjugate ocular torsion in the same direction as the tilt. Fundus photography can determine the different causes of ocular torsion and using the Parks-Bielschowsky three-step test (determining which eye is hypertropic, does the hypertropia increase in right gaze or left gaze and does the hypertropia increase with right or left head tilt) can also help differentiate OTR from SO palsy. The condition can improve or resolve after successful treatment of the underlying disease but, importantly, early diagnosis can be lifesaving, he said.
Patience is the word
Dr Julia Escardo-Paton then shared a case of ophthalmology taking “two steps forward, one step back”. There are patients who truly have it all and an 80-year-old man of Chinese ethnicity, was one such case, she said. With a long medical history, including previous bilateral medial orbital decompressions for optic neuropathy, he was referred by an orbital surgeon for ocular surface disease due to thyroid orbitopathy. He also had diplopia, glaucoma and hazy vision. The patient underwent squint surgery (6mm bilateral medial rectus recessions, R 4mm, L 5mm inferior rectus recessions, plus left temporary tarsorrhaphy) and later, bilateral cataract surgery. The surgeries, especially the first, were complex with a long recovery but ultimately the patient’s vision improved, intraocular pressure decreased (he came off his drops) and the ocular surface improved, said Dr Escardo-Paton. Lessons learnt included glaucoma drops with preservatives are toxic, large-angle squints can exacerbate ocular surface disease, tight muscles will cause secondary glaucoma and lagophthalmos and tight inferior recti preventing Bell’s reflex is a bad recipe for the ocular surface. Dr Escardo-Paton stressed the importance of explaining surgery’s limitations every step of the way, adding both surgeon and patient patience is a virtue!
Dr Penny McAllum discussed phlyctenular disease, typically affecting children (six months to 18 years). Often overlooked, it requires follow-up as left untreated it can lead to corneal ulceration, scarring and potentially vision loss. Phlyctenular disease is characterised by a hypersensitivity reaction of the cornea and conjunctiva to a bacterial antigen, most often staphylococcal, resulting in small, white/yellowish raised bumps (phlyctenules) that can move progressively towards the centre of the cornea if untreated. Common symptoms include light sensitivity, irritation, redness and blurred vision. Management involves topical antibiotic (Fucithalmic 2–3 times daily or chloramphenicol 4–6 times daily) and topical steroid (fluorometholone 2–4 times daily or prednisolone 2–4 times daily) or a combination treatment (Maxitrol four times daily). Patients, especially recurring cases, also benefit from blepharitis management, including hot compresses, eyelid massages and lid scrubs; non-preserved lubricant; omega-3 supplements; and oral azithromycin or doxycycline.
Dr Mark Donaldson then shared an intriguing case of Ehlers-Danlos syndromes (hereditary disorders of connective tissue with manifestations in all organ systems, including a wide range of eye issues), while Dr Arvind Gupta covered bitemporal hemianopia. Quite common, it is characterised by vision loss in the temporal half of both the right and left visual fields. A pathology of the optic chiasm, it is often associated with pituitary or suprasellar tumours, said Dr Gupta. While it is more likely a local than an intracranial cause, all these cases still require an MRI to rule out malignant tumours.
After a quick review of Pharmac’s ophthalmology pipeline (no good news) and a smorgasbord of cases, Dr Andrew Riley concluded the evening by thanking everyone for coming, particularly Prof Dai for making the trip from Brisbane. “It is a great honour to be back,” said Prof Dai. “Eye Doctors has a special place in my heart. Starting out, I recall going to talks with two optoms present. Look at you now – you’ve come a long way.”
Prof Dai also encouraged Kiwi eye health professionals to join him in Brisbane for the upcoming third Asia-Pacific Strabismus and Paediatric Ophthalmology Society (APSPOS) Congress from 29 June to 1 July 2025. For more, click here.