Approaches to dry eye diagnosis and management across the world
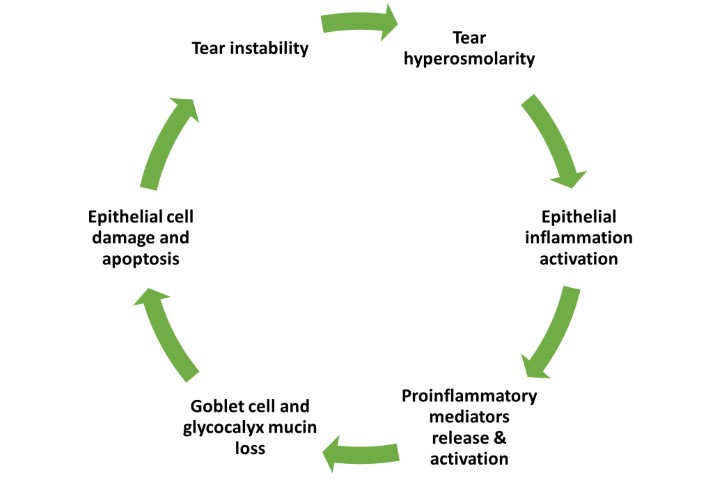
The Tear Film and Ocular Surface Society (TFOS) second Dry Eye Workshop (DEWS II) reports were published in 2017. These brought practitioners up to date on the evidence basis for dry eye disease (DED), including our current understanding of the pathophysiology, a consensus-refined definition and a more definitive approach to diagnosis, as well as outlining efficacious management options. However, in doing so, it also recognised the lack of published randomised clinical trials available to inform practitioners on how management options compare to one another at different levels of disease severity and across the spectrum of dry eye subtypes, from evaporative to aqueous deficiency. Hence an anonymous, cross-sectional online questionnaire (in Qualtrics) was administered to eyecare professionals around the world with the support of the TFOS ambassadors. Translated into 14 languages, this six-question survey sought to determine the management and treatment approaches taken by eyecare practitioners worldwide, based on disease severity and subclassification.
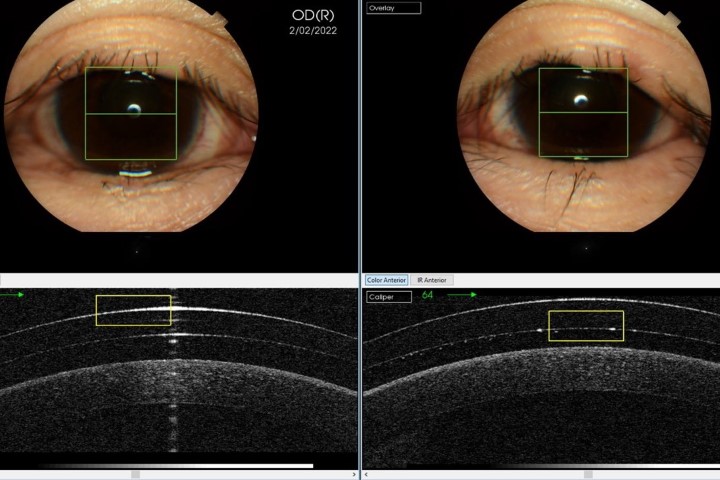
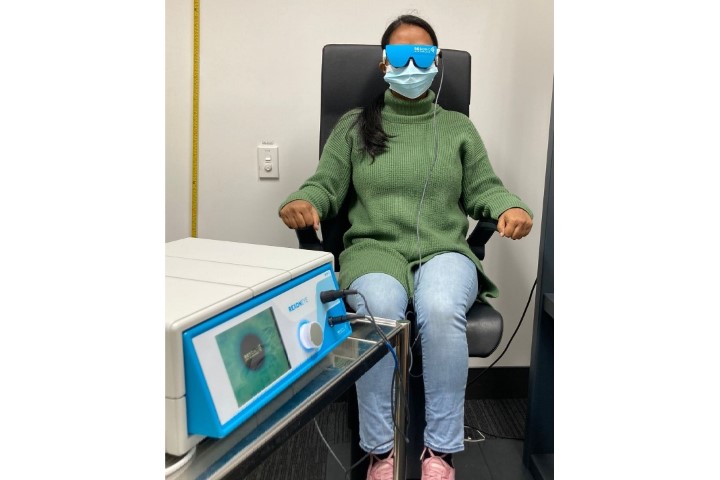
Completed by 1,139 eyecare professionals (37% ophthalmologists and 58% optometrists) from 51 countries1,2, the survey revealed that clinicians considered a wide range of diagnostic tools to be critical for a diagnosis of dry eye, the most common being verbal symptoms (69%), fluorescein breakup time (67%) and corneal staining (64%). In addition, reports of visual disturbance (57%), symptomology results from a validated questionnaire (48%), ocular redness (54%) and blink/lid closure analysis (54%) were commonly used to aid diagnosis. A median of seven tests was deemed essential to diagnose dry eye (range 0-28).
Tests which proved popular for differentiating dry eye subtypes were the Schirmer/phenol red thread test (32%), meibomian gland expression (32%) and orifice examination (32%), and blink/lid closure analysis (32%); use of verbal (38%) and questionnaire (30%) symptomatology, fluorescein breakup time (39%) and corneal staining (37%), for this purpose, were also noted. A wide range of management strategies were utilised at each severity level and across different dry eye subtypes. DED management and the treatments applied were identified to differ between continents and countries.
The survey was valuable in offering practitioners an opportunity to benchmark their current practice against regional and global norms and for identifying areas of research that might best inform future clinical practice. However, these data were collected in 2017-2018, when the TFOS DEWS II report had only recently been published. Therefore, a follow-up survey was recently launched to examine any changes in practice that might have occurred over the past five years. Data are currently being collated and the results will be analysed, interpreted and published, so watch this space for the outcomes!
References
- Wolffsohn J, Craig J, Jones L, Trave-Huarte S, Wang M. (2020) Global approaches to dry eye diagnosis. Invest. Ophthalmol. Vis. Sci. 2020;61(7):117.
- Wolffsohn J, Trave Huarte S, Jones L, Craig J, Wang, M and TFOS ambassadors. (2021) Clinical practice patterns in the management of dry eye disease: a TFOS international survey. Ocular Surface 21, 78-86.

Professor James Wolffsohn is head of the School of Optometry and the Department of Audiology at Aston University, UK, and a member of the TFOS board. He has research interests in ophthalmic instrumentation, myopia management, contact lenses, intraocular lenses and the tear film.

Professor Jennifer Craig heads the Ocular Surface Laboratory at the University of Auckland, is a member of the TFOS board and is the TFOS ambassador for New Zealand.