Ocular graft-versus-host disease – a model of severe dry eye
Ocular graft-versus-host disease (oGvHD) manifests in 60-80% of patients undergoing allogeneic haematopoietic stem cell transplantation, due to donor T cells incorrectly identifying recipient tissue as foreign, leading to an immunological attack by the donor cells1.
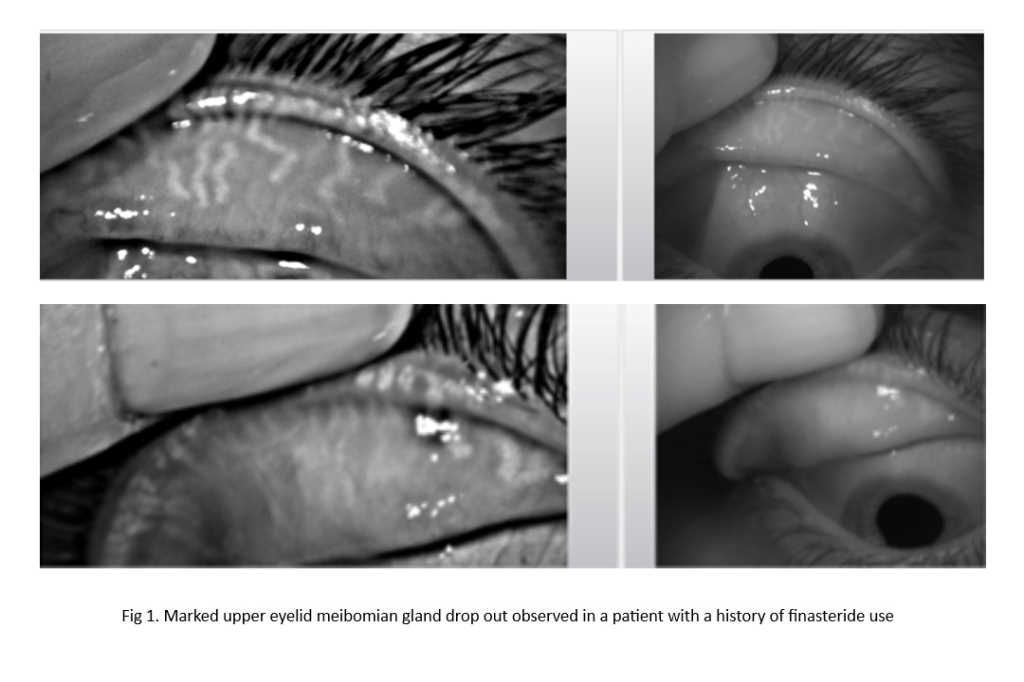
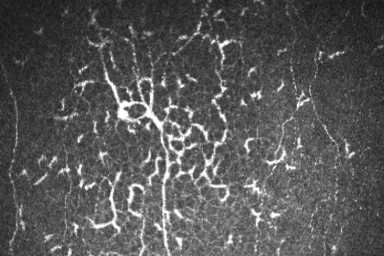
While acute oGvHD with an onset within the first month after transplantation is relatively rare (<10%), chronic oGvHD occurs in over 50% of patients within five to 25 months. The latter leads to severe dry eye disease (DED) with destruction of the lacrimal and meibomian glands as well as conjunctival scarring. As such, patients with oGvHD often present with myriad symptoms including blurred vision, light sensitivity, chronic conjunctivitis, burning and foreign-body sensation, itching and general eye pain2. Specific oGvHD diagnostic criteria include the Ocular Surface Disease Index (OSDI) questionnaire, Schirmer’s test, corneal fluorescein staining and conjunctival hyperaemia3.
Since inflammation of eyelids and lacrimal glands plays a major role in oGvHD, a more recent diagnostic approach includes the measurement of pro-inflammatory cytokines, such as vascular endothelial growth factor (VEGF), MMP-9, ICAM-1, IL-1β, IL-6 and IL-8, in tears. Inflammasome activation, which leads to an increase in these pro-inflammatory cytokines, has already been shown to be elevated in other DED forms4, with the inflammasome also reported to regulate acute GvHD5.
Current treatment options for oGvHD are limited and often insufficient, with strategies mainly aimed at tear preservation, lubrication and/or inflammation control using topical steroids or immunosuppressants such as cyclosporine1. However, these therapies are mostly targeted towards reducing specific symptoms rather than treating the underlying disease mechanism. As such, there is a need for novel therapies that act upstream in the inflammatory cascade, for example, by blocking inflammasome activation. However, to test such treatments, robust preclinical disease models are required.
As part of my Humboldt Fellowship, I’m currently working with Professor Philipp Steven at the University of Cologne. Prof Steven’s group has recently established a chemotherapy-based GvHD mouse model mimicking early onset of chronic oGvHD with characteristic signs of corneal epitheliopathy, lacrimal gland inflammation and blepharitis6. During my current visit, I’m investigating the involvement of the inflammasome in oGvHD by labelling ocular tissue sections for relevant markers. Subsequent visits in 2023 and 2024 will be used to test the efficacy of a novel inflammasome eye drop7, developed by the Buchanan Ocular Therapeutics Unit at the University of Auckland, to reduce oGvHD signs.
This research also forms part of a Health Research Council of New Zealand Project Grant, with the preclinical studies subcontracted to the University of Cologne. Receiving the Humboldt fellowship allows me to actively participate in the studies – a fantastic opportunity to learn new skills I can bring back to the University of Auckland. I am really enjoying my time with Steven’s team (pictured) and I am very excited about the potential impact of this research. Considering the increasing number of stem cell transplantations, the high prevalence of oGvHD and the severe impact on the ocular surface, I am very hopeful that our research will make a difference and reduce sight-threatening consequences associated with the disease.
References
1. Kezic J, Wiffen S, Degli-Esposti M. Keeping an 'eye' on ocular GvHD. Clin Exp Optom. 2022 Mar;105(2):135-142.
2. Dietrich-Ntoukas T, Cursiefen C, et al. Diagnosis and treatment of ocular chronic graft-versus-host disease: report from the German-Austrian-Swiss Consensus Conference on Clinical Practice in chronic GvHD. Cornea. 2012 Mar;31(3):299-310.
3. Kitko C, Pidala J, Schoemans H, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: IIa. The 2020 Clinical Implementation and Early Diagnosis Working Group Report. Transplant Cell Ther. 2021 Jul;27(7):545-557.
4. www.nzoptics.co.nz/articles/archive/inflammasome-markers-in-dry-eye-disease
5. Jankovic D, Ganesan J, Bscheider M, et al. The Nlrp3 inflammasome regulates acute graft-versus-host disease. J Exp Med. 2013 Sep 23;210(10):1899-910.
6. Gehlsen U, Stary D, Maass M, et al. Ocular graft-versus-host disease in a chemotherapy-based minor-mismatch mouse model features corneal (lymph-) angiogenesis. Int J Mol Sci. 2021 Jun 8;22(12):6191.
7. www.nzoptics.co.nz/articles/archive/non-aqueous-eye-drops-friend-or-foe

A/Prof Ilva Rupenthal is the director of the Buchanan Ocular Therapeutics Unit (BOTU) in the Department of Ophthalmology at the University of Auckland.