The effect of an astaxanthin-based dietary supplement on dry eye disease
In Covid-affected 2021, three BOptom students joined the OSL team to explore the effects of an oral astaxanthin (AXT)-based supplement under the supervision of Professor Jennifer Craig, Dr Alex Muntz and myself. The team recruited 30 participants with mild-to-moderate dry eye disease (DED), who took two capsules/day (12mg AXT total) of the supplement for 90 days.
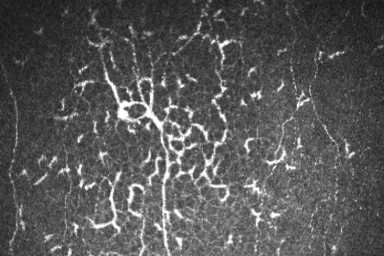
AXT is a red-pigmented marine carotenoid closely related to lutein and zeaxanthin1 and farmed from the freshwater microalgae Haematococcus pluvialis. Its unique molecular structure allows it to span cell membranes, which is understood to confer significant medical advantages, especially when targeting inflammation, apoptosis and oxidative damage2. A number of studies have shown AXT potentially offers protection against a number of ocular diseases including dry age-related macular degeneration (AMD), diabetic retinopathy and glaucoma3. Because DED involves an ocular surface inflammatory component4, we wanted to know whether the oral AXT-based capsule might reduce signs and symptoms of DED.
Asta Supreme Advanced Vision Care is marketed as a nutraceutical for AMD patients. Table 1 lists the capsule contents. Although AXT is a key ingredient, the complex nature of the product precludes attributing any benefits solely to AXT.
Study method
After becoming proficient in the use of the Oculus Keratograph K5, slit lamp techniques and administration of dry eye questionnaires, the OSL AXT research students gathered objective and subjective data over three months in the form of in-clinic baseline testing at day 0 and re-testing at day 90. Electronic DED questionnaires were also completed at days 0, 30, 60 and 90. Parametric and non-parametric data analysis allowed comparisons of quantitative and qualitative measures obtained at different timepoints of the study. Tables 2 and 3 summarise the study parameters measured.
Results
Unfortunately, clinical results requiring on-site measurement were impacted by Covid disruptions, so disappointingly only eight of the 30, 90-day final clinical assessments could be completed in person. Following statistical correction that had to be applied to account for the small sample size (requiring p to be <0.01, rather than the usual 0.05), it was pleasing to confirm a significant reduction in tear osmolarity in the right eye (p=0.008). Supporting the change in clinical signs were alterations in the electronic questionnaire responses for the full cohort, which highlighted a statistically significant improvement in DED symptoms, based on OSDI scores at days 60 and 90 (p<0.01 in both cases). OSDI subscale analysis showed dry eye symptoms (but not vision-related function or susceptibility to environmental triggers) to be significantly reduced by days 60 and 90 (p=0.008). SPEED questionnaire scores also dropped at days 60 and 90 but not significantly (p=0.03).
Discussion
There is a growing body of evidence that AXT’s potent antioxidant and anti-inflammatory effects have the potential to reduce the levels of pro-inflammatory cytokines and reactive oxygen species in tears5. Since tear hyperosmolarity is considered an important biomarker for DED6, along with the OSDI score, these preliminary findings suggest exploration of the product for DED is warranted. A well-designed, randomised, double-masked clinical trial, involving a larger sample size, a wider age range than the predominantly university-aged cohort in the pilot study, full objective clinical follow-up for at least 90 days and a placebo control, could establish the benefits attributable directly to AXT.
References
- Ambati R, Phang S, Aswathanarayana R. Astaxanthin: sources, extraction, stability, biological activities and its commercial applications- a review. Mar Drugs 2014; 12: 128-152.
- Fakhri S, Abbaszadeh F, Dargahi L, Jorjani M. Astaxanthin: A mechanistic review on its biological activities and health benefits. Pharm Res 2018; 136: 1-20.
- Giannaccare G, Pellegrini M, Senni C, Bernabei F, Scorcia V, Cicero A. Clinical applications of astaxanthin in the treatment of ocular diseases: emerging insights. Mar Drugs 2020; 18: 239
- Craig J et al. TFOS DEWS II definition and classification report. Ocul Surf 2017; 15: 276-283.
- Huang J-Y, Yeh P-T, Hou Y-C. A randomised, double blind, placebo-controlled study of oral antioxidant supplement therapy in patients with dry eye syndrome. Clin Ophthal 2016; 10: 813-820.
- Suzuki M, et al. Tear osmolarity as a biomarker for dry eye disease severity. Invest Ophthalmol Vis Sci 2010; 51: 4557-4561.

Grant Watters is an adjunct academic in the School of Optometry and Vision Science and the Department of Ophthalmology at the University of Auckland and the clinical director of Mortimer Hirst Optometrists in Auckland.