Paediatric dry eye
The misconception that dry eye disease (DED) primarily affects the elderly presents a risk of overlooking issues in children. DED has been reported in paediatric populations with a prevalence of up to 33%1. As in adults, risk factors for paediatric DED include diabetes, Sjögren’s syndrome, blepharokeratoconjunctivitis, allergies, contact lenses and the use of digital screens.
The TFOS DEWS II diagnostic criteria for DED require a patient to be symptomatic and exhibit a clinical sign indicating loss of ocular surface homeostasis2. To be positive for symptoms, this requires either an Ocular Surface Disease Index (OSDI) score of ≥13 or a Dry Eye Questionnaire 5 (DEQ-5) score of ≥6. As paediatric patients aren’t always able to communicate their symptoms, researchers in Sydney have looked at the use of dry eye symptomology questionnaires in patients between the ages of six and 15 years of age3. They found the DEQ-5 and Instant Ocular Symptoms Survey (IOSS) showed reasonable repeatability and best suited patients in this age group as the use of simpler language required less assistance from the clinician. Outcomes were not assessed relative to objective signs of DED, however, to be able to infer relative clinical validity of the questionnaires in this age group.
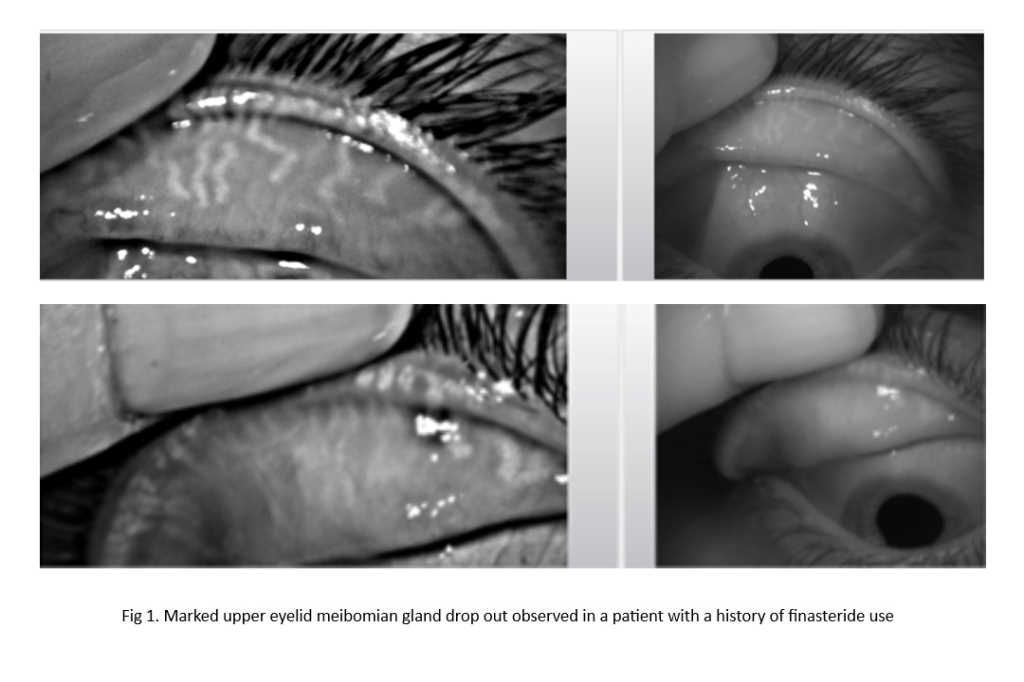
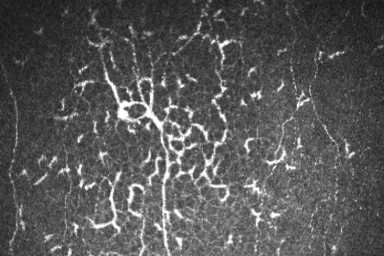
The literature suggests paediatric ocular surface assessment is generally similar to that of adults. Tear breakup time using non-invasive equipment such as the Oculus Keratograph 5M is well tolerated by children4. However, in practices without such equipment, minimal amounts of fluorescein can be used to assess tear film stability. It should be noted that the tear film breakup time in children without dry eye disease is typically higher than that of adults without dry eye disease5, raising the question of whether diagnostic thresholds for clinical tests need to be reviewed and redefined for the paediatric population. Other tests, such as measurement of tear film osmolarity, assessment of tear volume, meibomian gland evaluation and ocular surface staining have all been performed safely in children, although age-specific differences in diagnostic cut-off values are yet to be agreed.
Published randomised controlled trials assessing dry eye treatments in children are lacking. Given the established safety and efficacy of environmental modification advice, artificial tears and warm compresses in adults6 – and without evidence to the contrary in paediatric patients - treatment approaches tend to be similar in children. Therapeutic options reserved for moderate-to-severe forms of dry eye disease, such as topical and oral antibiotics, anti-inflammatories and amniotic membrane transplants also lack comprehensive evaluation of efficacy in paediatric populations. Risks associated with tetracycline preclude the use of doxycycline in children whose adult teeth are not fully developed.
In summary, clinicians should be mindful of the risk factors associated with DED and perform tests as necessary to identify affected children. Research to confirm safety and efficacy of existing treatments in this age group is warranted to aid practitioners in selecting the most appropriate therapies.
References
1. Rojas-Carabali W, et al. High prevalence of abnormal ocular surface tests in a healthy pediatric population. Clin. Ophthalmol. 14, 3427–3438 (2020).
2. Wolffsohn J, et al. TFOS DEWS II Diagnostic Methodology report. Ocul. Surf. 15, 539–574 (2017).
3. Chidi-Egboka N, Golebiowski B, Lee S, Vi M, Jalbert, I. Dry eye symptoms in children: can we reliably measure them? Ophthalmic Physiol. Opt. 41, 105–115 (2021).
4. Xie W, et al. Assessment of tear film and bulbar redness by Keratograph 5M in pediatric patients after orthokeratology. Eye Contact Lens 44, S382–S386 (2018).
5. Chidi-Egboka N, Briggs N, Jalbert I, Golebiowski B. The ocular surface in children: A review of current knowledge and meta-analysis of tear film stability and tear secretion in children. Ocul. Surf. 17, 28–39 (2019).
6. Jones L, et al. TFOS DEWS II Management and Therapy Report. Ocul Surf vol. 15 575–628 (2017).

Bhavna Patel is an optometrist and professional teaching fellow at the University of Auckland’s School of Optometry and Vision Science. She has a special interest in dry eye and is currently completing a clinical master’s degree under the supervision of Professor Jennifer Craig and Dr Phil Turnbull.