The current state of ocular surface pain and its future
Ocular surface pain is a leading cause of eyecare visits and healthcare costs, having an observable negative impact on quality of life1. As a consequence of both ocular and systemic disorders, and driven by various mechanisms that are often difficult to fully elucidate, ocular surface pain is often ignored or not fully addressed2. However, given the prevalence and morbidity of the disorder, it is important to understand the current state of the field and potential future directions.
Examining ocular surface pain
In recent years, it has been acknowledged that ocular surface pain can have multiple contributors, potentially being driven by nociceptive (pain that arises from actual or threatened damage to non-neural tissue3), neuropathic (dysfunction within the somatosensory nervous supply to the ocular/periocular regions), or mixed mechanisms4. Potential nociceptive sources of pain include abnormal tear quantity and composition, anatomic abnormalities and environmental exposures. Potential neuropathic contributors are nerve abnormalities anywhere in the pathway that connects the ocular surface to the brain, and thus can include both peripheral and central nerve defects.
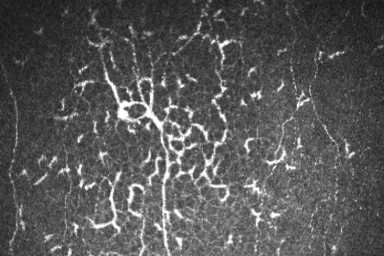
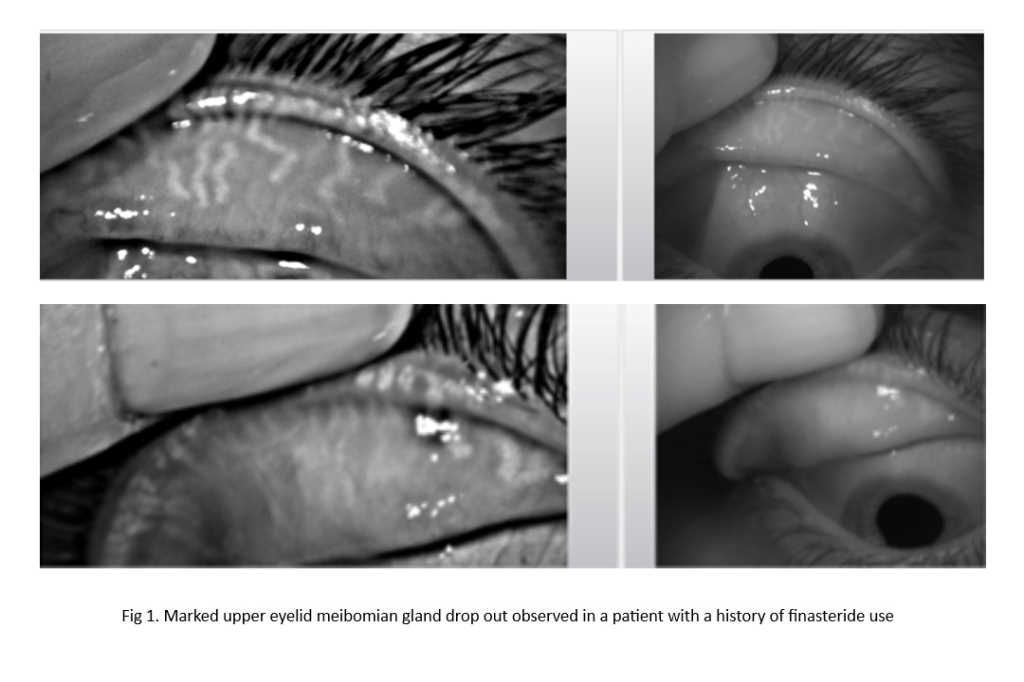
A quick but comprehensive examination is needed to identify potential contributors to ocular surface pain. This includes standardised questionnaires that quantify the severity of pain and give information on its characteristics. Dry-eye-specific questionnaires can be administered that have pain questions included, such as the 5-item Dry Eye Questionnaire (DEQ5)5 and Ocular Surface Disease Index (OSDI)6, or pain-specific questionnaires can be used, such as the Ocular Pain Assessment Survey (OPAS)7 and Neuropathic Pain Symptom Inventory-modified for the Eye (NPSI-E)8. Also important is obtaining information on the patient’s systemic co-morbidities and medications. Next, an examination looking for nociceptive sources of pain should be conducted, looking for evidence of ocular surface inflammation (presence of bulbar injection, InflammaDry (Quidel) positivity, low tear production, tear film instability, meibomian gland abnormalities and epithelial cell disruption, to name a few. Incorporated within the examination is an assessment of metrics that suggest a neuropathic contribution to pain, including abnormal corneal sensitivity, persistent pain after an anesthetic eye drop and nerve abnormalities on confocal microscopy.
Overall, findings that suggest a neuropathic contribution to pain include: symptoms out of proportion to examination findings; specific symptom descriptors of pain evoked by wind and light; presence of systemic pain co-morbidities, such as migraine and fibromyalgia; abnormal corneal sensitivity (either hyper- or hypo-sensitivity); persistent pain after instilling anaesthetic drops; and presence of cutaneous allodynia (pain to light touch of the skin around the eye)2. The latter two findings are more suggestive of a central neuropathic component to pain.
Managing ocular surface pain
Possibly most important, however, is our rapidly expanding toolbox to manage ocular surface pain. In cases of nociceptive pain, nociceptive sources need to be addressed. Anti-inflammatory agents such as cyclosporine or lifitegrast9 are often used, especially in individuals with systemic immune disorders. Fewer studies have focused on the treatment of neuropathic pain; however, establishing the likely location of the nervous lesion via the aforementioned process can help to guide the therapeutic ladder.
Patients with peripheral neuropathic pain (neuropathic features but pain is relieved with topical anesthetic) often improve with topical anti-inflammatories and growth-factor-containing blood products (such as autologous serum tears, platelet-rich plasma10), and there is excitement about potential new therapies, such as recombinant nerve growth factor11 and transient receptor potential cation channel subfamily V member 1 (TRPV1) antagonists12, among others. In comparison, oral neuromodulators, like α2δ ligands, antidepressants and anticonvulsants have been successfully used in individuals with central neuropathic pain13. Opioid-based agents such as naltrexone14 and adjuvant therapies such as nerve blocks15, botulinum toxin injections16, or external neurostimulation devices17, are also growing in use. Because these agents are not direct analgesics, pain relief can take months, often mandating combination therapy and proper counselling on expectations.
The future
Our knowledge of ocular surface pain is continuously evolving and it is important to highlight the key strides that have been made. For example, the discovery of various underlying phenotypes has allowed us to treat pain more effectively. However, our current diagnostic armamentarium is limited and new diagnostic tests are needed to better categorise patients with respect to their peripheral and central nerve status. Furthermore, new mechanism-specific therapies are needed, especially topical therapies that can decrease pain without inducing significant side effects, such as corneal anaesthesia.
Our goal is to deliver precision-based therapy that targets both nociceptive and neuropathic abnormalities in an individual patient to reduce pain and improve quality of life. Beyond treatment, an additional goal is prevention, identifying individuals at risk of ocular surface pain development (for example, after a surgical procedure) and intervening appropriately. Research into understanding genetic and epigenetic contributors to pain may help in this regard and gene-modulating therapies may prove to be breakthroughs in this field.
References
1. Patel S, Felix E, Levitt R, et al. Dysfunctional Coping Mechanisms Contribute to Dry Eye Symptoms. J Clin Med 2019;8(6).
2. Mehra D, Cohen N, Galor A. Ocular Surface Pain: A Narrative Review. Ophthalmol Ther 2020;9(3):1-21.
3. IASP terminology. Accessed June 2022.
4. Dieckmann G, Goyal S, Hamrah PJO. Neuropathic corneal pain: approaches for management. 2017;124(11):S34-S47.
5. Chalmers R, Begley C, Caffery B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Cont Lens Anterior Eye 2010;33(2):55-60.
6. Schiffman RM, Christianson M, Jacobsen G, et al. Reliability and validity of the Ocular Surface Disease Index. Arch Ophthalmol 2000;118(5):615-21.
7. Qazi Y, Hurwitz S, Khan S, et al. Validity and Reliability of a Novel Ocular Pain Assessment Survey (OPAS) in Quantifying and Monitoring Corneal and Ocular Surface Pain. Ophthalmology 2016;123(7):1458-68.
8. Farhangi M, Feuer W, Galor A, et al. Modification of the Neuropathic Pain Symptom Inventory for use in eye pain (NPSI-Eye). Pain 2019;160(7):1541-50.
9. Mehra D, Cohen NK, Galor AJO, Therapy. Ocular surface pain: a narrative review. 2020;9:1-21.
10. Aggarwal S, Kheirkhah A, Cavalcanti B, et al. Autologous Serum Tears for Treatment of Photoallodynia in Patients with Corneal Neuropathy: Efficacy and Evaluation with In Vivo Confocal Microscopy. The Ocular Surface 2015;13(3):250-62.
11. Sacchetti M, Lambiase A, Schmidl D, et al. Effect of recombinant human nerve growth factor eye drops in patients with dry eye: a phase IIa, open label, multiple-dose study. British Journal of Ophthalmology 2020;104(1):127.
12. Fakih D, Guerrero-Moreno A, Baudouin C, et al. Capsazepine decreases corneal pain syndrome in severe dry eye disease. J Neuroinflammation 2021;18(1):111.
13. Patel S, Mittal R, Felix E, et al. Differential Effects of Treatment Strategies in Individuals With Chronic Ocular Surface Pain With a Neuropathic Component. Frontiers in pharmacology2021; v. 12.
14. Jackson D, Singh S, Zhang-James Y, et al. The Effects of Low Dose Naltrexone on Opioid Induced Hyperalgesia and Fibromyalgia. 2021;12:136.
15. Small L, Galor A, Felix E, et al. Oral Gabapentinoids and Nerve Blocks for the Treatment of Chronic Ocular Pain. Eye Contact Lens 2020;46(3):174-81.
16. Diel R, Kroeger Z, Levitt R, et al. Botulinum Toxin A for the Treatment of Photophobia and Dry Eye. Ophthalmology 2018;125(1):139-40.
17. Mehra D, Mangwani-Mordani S, Acuna K, et al. Long-Term Trigeminal Nerve Stimulation as a Treatment for Ocular Pain. Neuromodulation 2021;24(6):1107-14.

Dr Sneh Patel is a recent graduate of the University of Miami Miller School of Medicine. His research focus is chronic ocular disorders such as dry eye disease, with a specific interest in the evaluation and treatment of acute and chronic ocular pain. He is pursuing a residency in physical medicine and rehabilitation at the VA-UCLA Medical Center in Los Angeles, CA, after which he hopes to complete a fellowship in interventional pain medicine.

Dr Anat Galor is a cornea and uveitis-trained specialist with dual appointments at the Miami Veterans Affairs (VA) Medical Center and the Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. She runs the ocular surface programme at Miami VA and has focused her research on the mechanisms underlying chronic ocular surface pain, with an emphasis on studying new diagnostic and treatment modalities.
Research is supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences R&D, Biomedical Laboratory R&D, Rehabilitation R&D, Department of Defense Gulf War Illness Research Program and Vision Research Program, National Eye Institute, NIH Center Core Grant and Research to Prevent Blindness.